One ongoing balancing act in benefits is the line between member experience and cost management. To be successful, it’s important to create strategies specifically for high utilizers of care.
Why? Because their benefit elections and usage can have an outsize impact on your financials and workload.
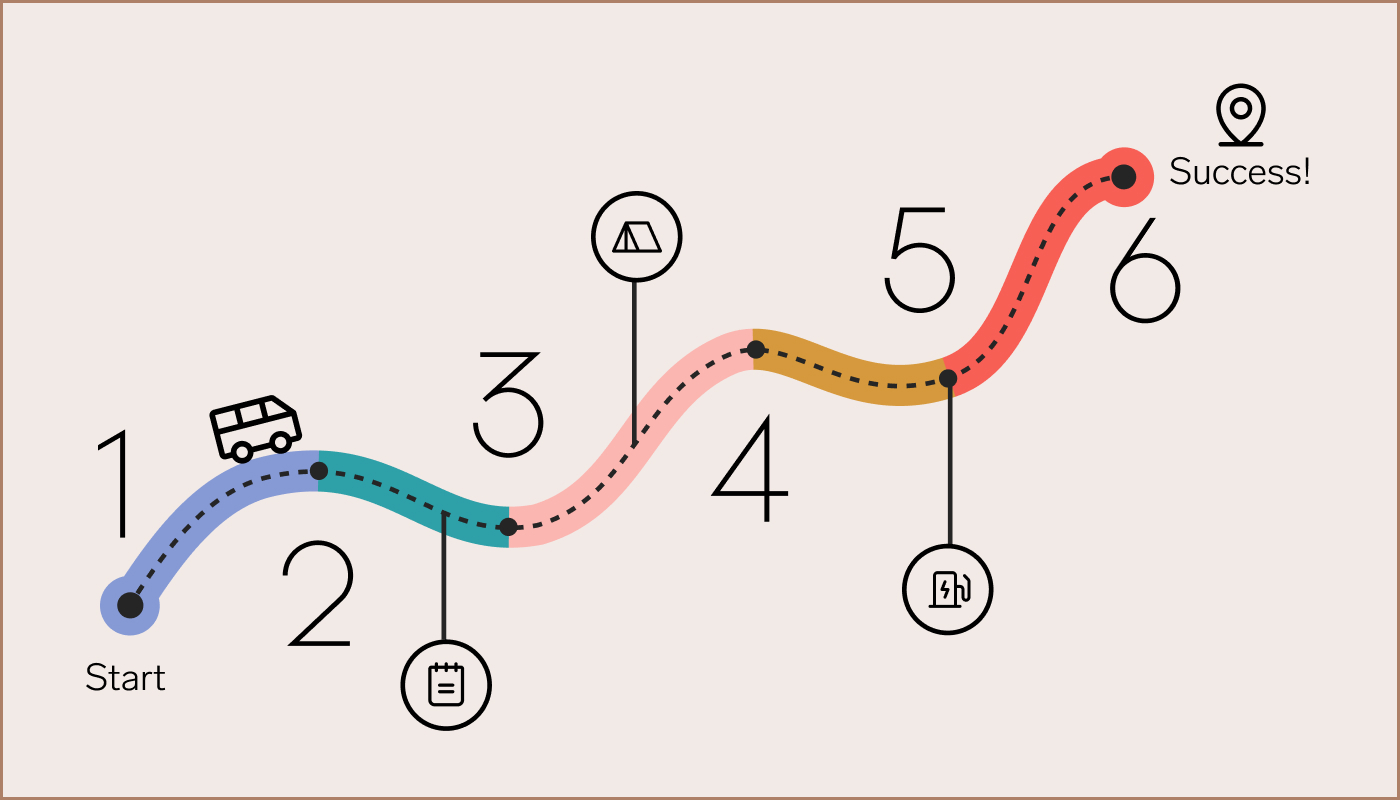
Here are ways to get ahead of it during Open Enrollment:
- In your OE communications, remind employees to think about their needs for the whole year. Calling out specific situations—like pregnancy, diabetes, or asthma—can help employees realize what they need to plan for this year. Then, direct them to resources like Q&A sessions, online chat, or office hours, to get the personalized context they need.
- Pull a report to identify high-cost claim trends from this year and prior years. Be sure to leave out any personal identifiable information and focus on the top situations or conditions likely to impact the company.
- Categorize your population’s needs and usage, to identify trends and unique characteristics. That could include:
- Telehealth or alternative location offerings
- Fertility support
- Maternity support
- Chronic health conditions: This can range from second opinions to caregiver services.
- Behavioral health: This can range from sleep, stress, or mood disorders to substance-use disorders, autism, or developmental needs.
- Partner with your broker/consultant and internal team to find value-added offerings, based on those needs. While it may be too late to redesign your plan for this year, your existing health plan or provider may offer ways to address these needs. Finding out during OE allows you to guide these high-need employees toward specific plans, if the offerings are tied to them.
- Consider building a worksheet that allows employees to enter in info on their needs and get the estimated costs for each offered plan. Your finance team or broker/consultant can help with this—or your health plan partner may already provide it.
- Plan to allocate dollars toward year-long education campaigns about the savings from getting pre-authorizations or price-checking before procedures.
Your employee experience matters all year long, not just during Open Enrollment.
See how leading companies are doing it differently, in a new Harvard Business Review Analytic Services report.
Get the report