Have you ever caught yourself thinking, “I’d love to turn on a few new innovative programs, but every new program creates a lot of new work for my team.”
You aren’t alone. This is a big problem for employers. We call it the innovation tax.
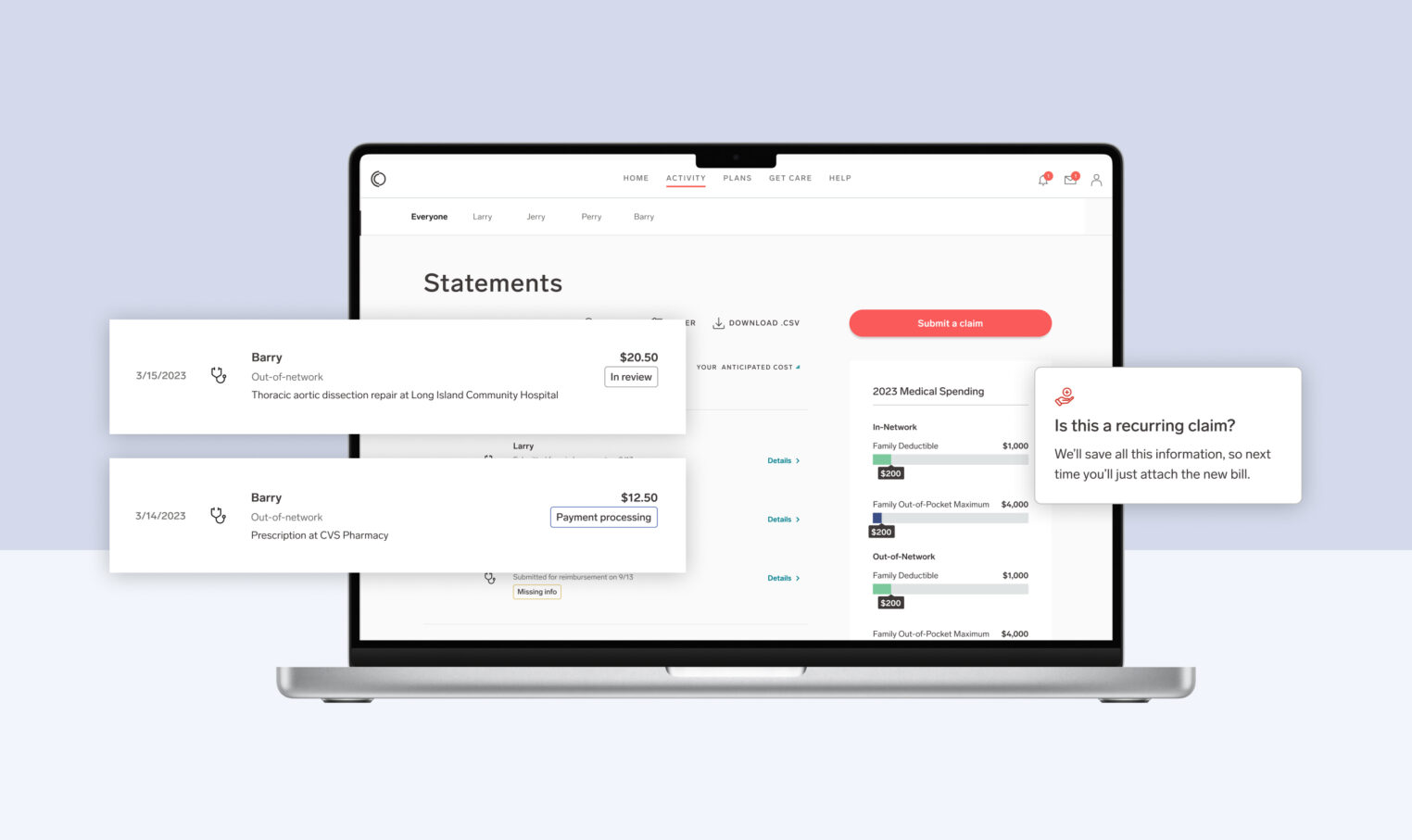
What used to take us four hours now takes us five minutes.
At Collective Health, we set out to lower this tax by building new technology that allows our clients to (almost) effortlessly turn on new programs. Our latest launch is a huge step in the right direction.
Why are new integrations difficult? They require a giant game of telephone
Data inaccuracy is one of the biggest and least talked about problems in our industry. Take eligibility data as an example.
When a member goes to see their provider, they expect the provider to be able to confirm their coverage. Any problems can lead to delays or even denials of needed care. Unfortunately, traditional health insurance is full of eligibility problems which trigger an extremely frustrating series of calls—between members, benefits teams, health plans, providers, and others—just to get basic issues resolved.
Why is this such a problem? It can be traced back to a large-scale game of data telephone. In order to get eligibility data from an employer to a provider, files are passed through multiple partners and systems, most often through the transfer of (very old school) EDI 834 files. With each layer of telephone, partners interpret and change the data to meet their needs. So with every transfer, we inevitably get data degradation.
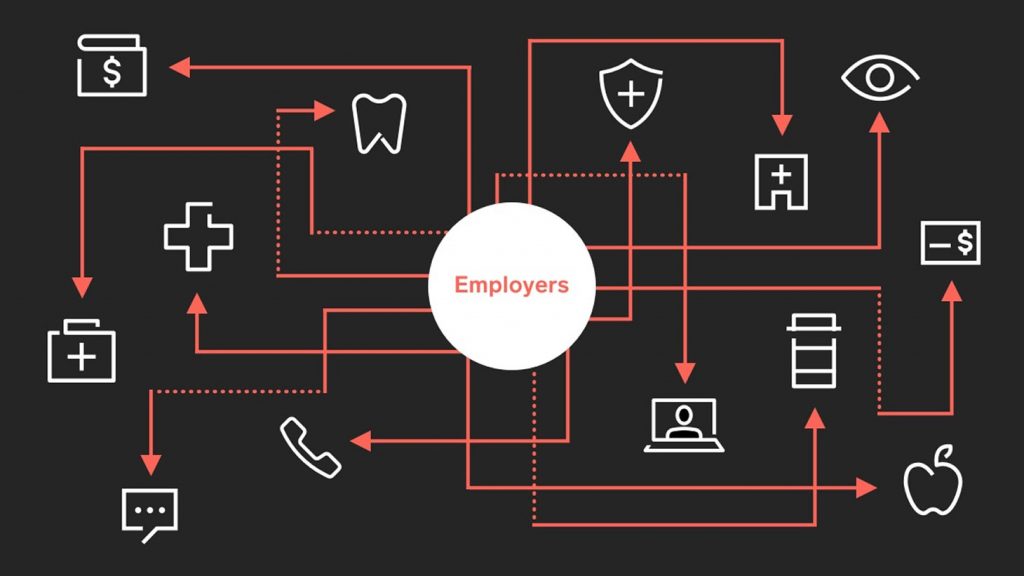
To make matters worse, integrating with each partner’s specific file requirements takes a significant amount of time to not only set up, but also maintain. Given each partner’s unique file format, it can take hours to manually check for and clean up information that may have been lost in translation during the integration process. Plan administrators, benefits leaders, and partners all have to spend time troubleshooting these issues, taking them away from more strategic activities.
Introducing Collective Health’s Eligibility Management Tool
At Collective Health, we believe that manual error checking and time-consuming integrations shouldn’t be accepted in this day and age. Industries with a high reliance on data accuracy, like banking and finance, have seen rapid process automation lead to improved accuracy. It’s time to expect the same of our healthcare systems.
We’ve developed a new eligibility file tool that seamlessly supports the specifications of program partners on the Collective Health platform. We can now give partners the data they need, without having to go through multiple layers of manual setup and maintenance.
Basically, we’re aiming to destroy the game of telephone.
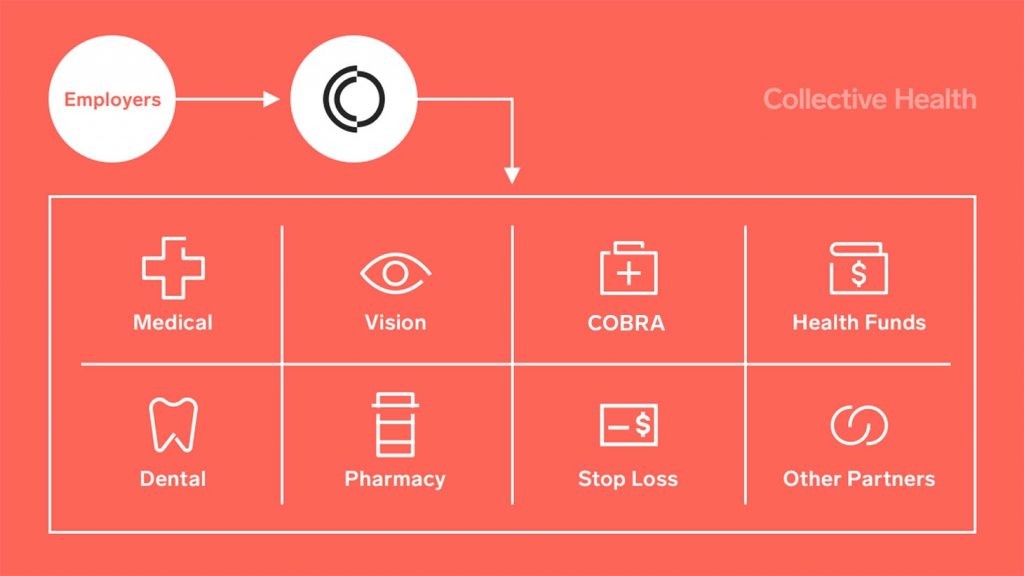
This technology makes it easier, faster, and cheaper to setup and maintain new integration files, and it makes the data accurate and reliable, too.
Integrations made 98 percent easier
Before we built this tool, it took us about four hours to complete program partner eligibility file set-up processes for every new program a client put in place.
Now, it only take us five minutes.
Why should you care that we eliminated 98 percent of the work?
When we spend less time setting up files, we can focus more resources on building powerful new member and client-facing features. Plus, with more accurate data and less error-prone manual integrations, you, your members, and your partners have to spend less time troubleshooting issues and fixing problems. Everyone benefits.
A seamless future for health insurance
This work is the first step toward smarter industry standards and technologies. While we’re starting with program partners, we also aim to simplify network partner integrations too. In creating new processes and tooling to make data sharing between health entities quicker, easier, and less manual, we can drive toward a standard data language with more seamless translations—empowering decades of employer-driven innovation.
Ultimately, we want to cut the innovation tax to zero. When we do that, we all win.