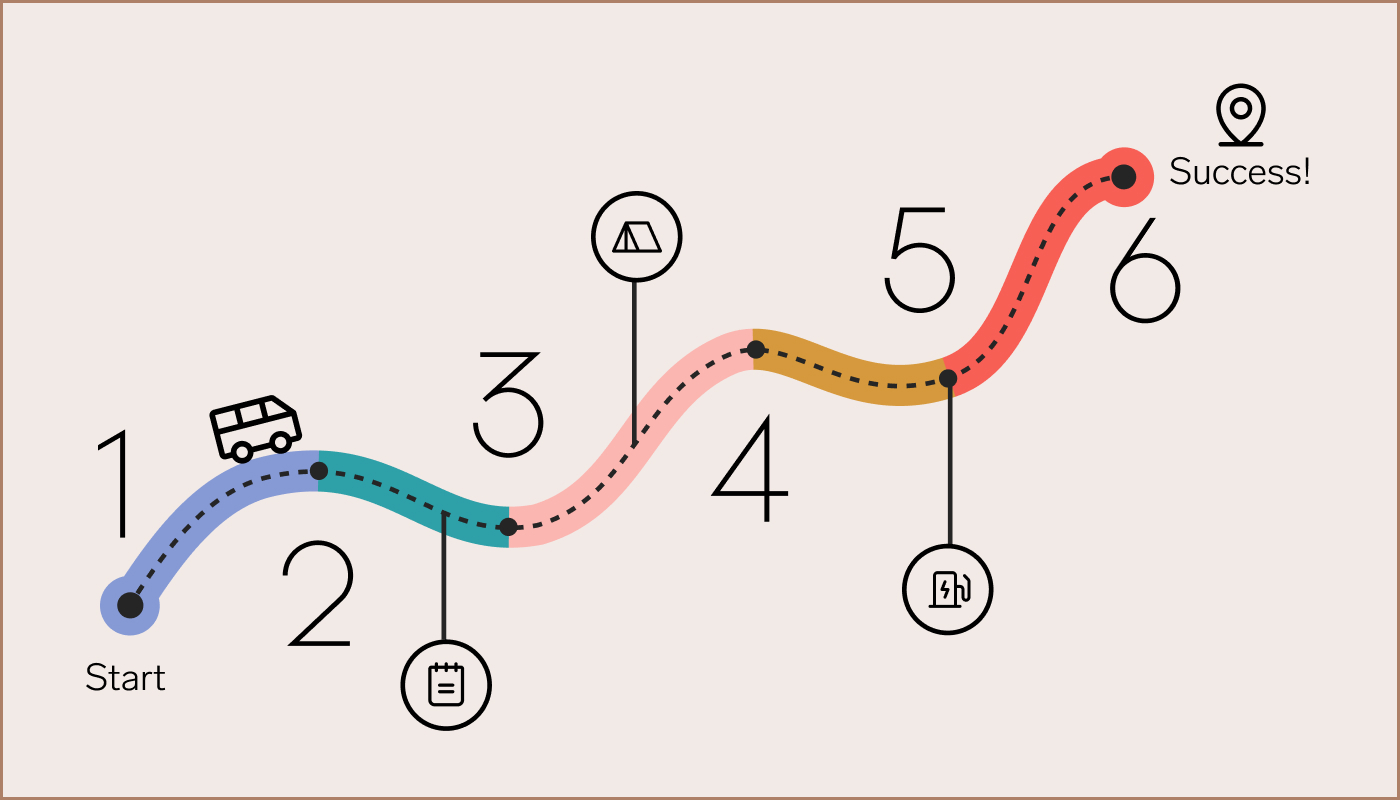
When your company changes medical networks, it is often an opportunity to upgrade care for your people. But, the transition to a new network can be challenging and confusing—for your benefits team as well. With careful preparation, expert advice, and clear communication, you can ensure a more seamless experience for everyone.
The more confident your team is during the process, the easier it is to help your people see the change as a positive one.
Start with your team
Make sure your benefits team has adequate time prior to the Open Enrollment period to review all plan documentation and any tools provided by the network. Encourage them to prepare for the questions they’ll likely get from your people during the transition. The more confident your team is during the process, the easier it is to help your people see the change as a positive one.
Introduce the new network to your people (with snacks)
- Plan an in-person benefits fair before Open Enrollment. Bring in representatives from your new network for a meet and greet, and serve healthy snacks. Everyone needs a snack break now and then.
- Work with your network partner to open their phone lines for Open Enrollment ahead of time. Your people are busy and will appreciate the extra time to get important coverage questions answered before they commit to specific plans.
- Provide your people with any search tools the network partner offers so they can determine if their providers are in-network. If the network does not provide a search tool, guide your people to call their doctors’ offices directly to confirm coverage.
Share the following “pro tips” with your people to help them with the transition
Share these tips—and other expert advice you’ve gleaned over the years—in your Open Enrollment presentations, on your internal wiki or intranet, or at in-person meetings before the transition. Many of these tips are also useful for people who are just making a plan change and not a full network change.
- Understand how the network change may impact upcoming care and life events. If you’re having a baby, need dental surgery, are considering behavioral or physical therapy, or are overdue for an eye exam, make sure you’re exploring the plan that will best fit you within the new network.
- Avoid care interruptions. If you’re currently in treatment with a provider who is out-of-network on your new plan, check to see if your new health insurance offers a Continuity of Care program. You’ll probably have to apply, but if your application is approved you’ll be able to finish your treatment with your out-of-network provider at in-network rates.
- Avoid medication interruptions. Refill your prescriptions one last time before your plan changes to make sure you have an adequate supply of each medication before you move to the new plan. If you have trouble filling a prescription on your new plan, contact your new network rather than paying out-of-pocket. Your new plan may have new rules, such as only covering generic equivalents for certain drugs, and your pharmacist may not have those details available.
- Prior authorization transfers. Many kinds of medical and pharmaceutical treatments require prior authorization. If you’ve been through this process on your current plan, work with your new insurance and/or your provider to reinitiate the prior authorization process. Generally, if you are on a January 1st start date for your new plan, December or January are the best times to do this.
- Contact your case manager. If you are in case management, typically your new health plan will give you a call in December or January to assign you a new case manager. So, if you see a call from a number you don’t recognize, you might want to answer it! If you don’t hear from your new insurance, you can contact them directly to request case management.
Network changes often go hand-in-hand with upgraded offerings for your people. So it is important that your team can ensure that your people have the information they need to complete the network change process quickly, easily, and without care interruptions. That way, not only can you ensure that your network change will go smoothly, but that any upgrades you are making to take better care of your people are appreciated.