When we think about nearly every aspect of our daily lives, from grocery shopping to banking to picking up a cup of coffee, the technology benefits are obvious — easy access to information, visibility into payments, automated alerts, and everything at the touch of a finger. The healthcare industry, historically, lags behind technologically to the detriment of both members and health benefits leaders. Only 12% of Americans have proficient health literacy, or the ability to obtain, process, and understand basic health information to make informed decisions. Benefits leaders are stuck working in disconnected, archaic operating systems with little clarity on the overall success of their health plans.
Healthcare’s outdated and disjointed landscape can greatly benefit from modern technology, but there are a few things that stand in its way.
1) Legacy Technology
To more seamlessly integrate technology, the systems healthcare runs on need to change. U.S. healthcare operates on legacy information systems, fax machines, and 30 year-old software that format data in ways that are error-prone and non-descriptive. Most of today’s new digital health solutions are simply layered on top of this legacy technology, meaning the systems don’t often communicate well with one another. When it comes to employer healthcare, the result is a healthcare experience that’s confusing, fragmented, costly, and benefits leaders don’t have access to, nor a clear understanding of how their benefits programs are working for their people.
How we can help:
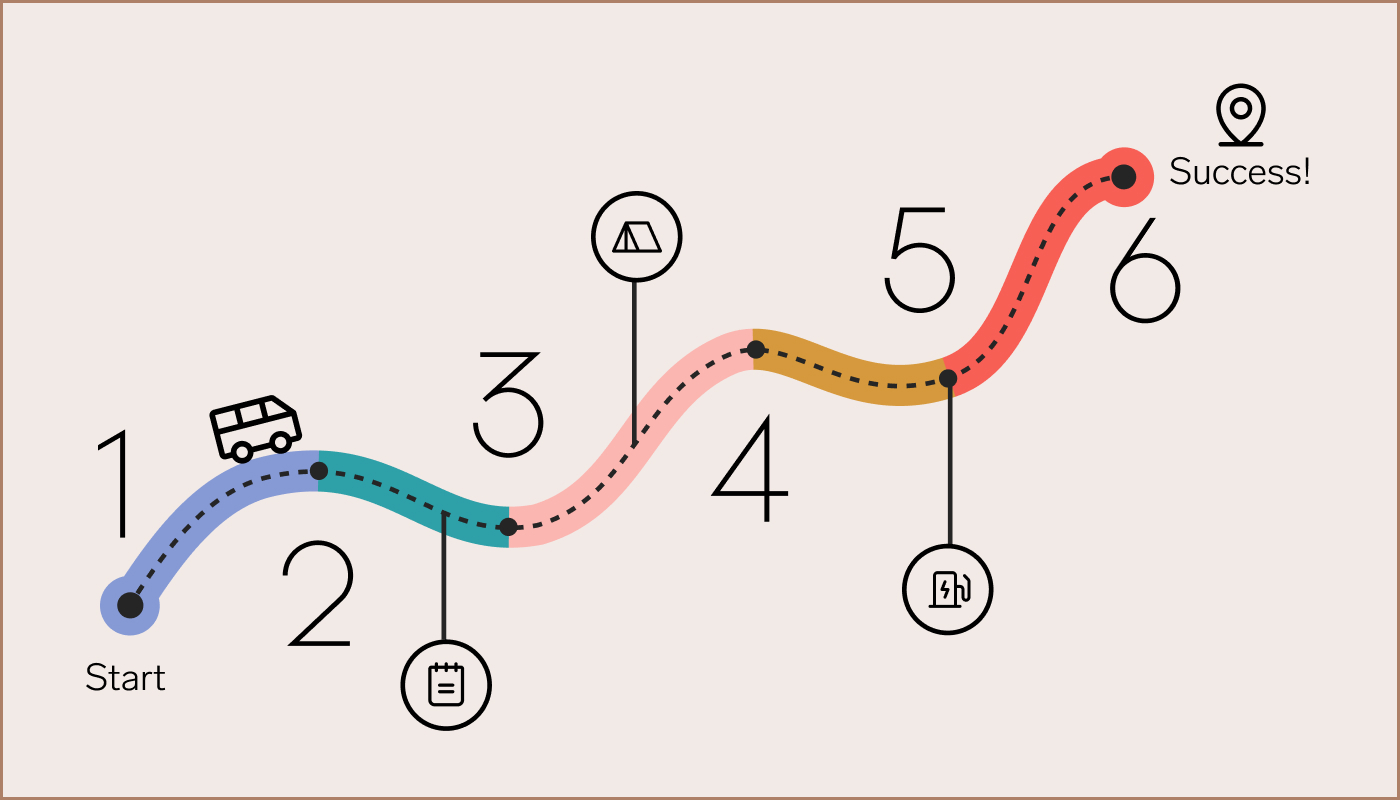
At Collective Health, we’ve launched Collective Compass™, a suite of products and services that simplifies how employers and consultants manage their full healthcare strategy—all from one convenient, connected platform. The platform is built to allow for clear communication between all of the moving pieces of your health plan, so they work together more seamlessly. Just one example of how we connect your strategy is with our FMP (financial management and payments). We gather claims payments from your medical, dental, pharmacy, and vision networks, along with anywhere from three to ten partner solutions, and funnel them into one, simple payment (portal, system). Read more here.

2) Limited Transparency
Most benefits leaders have limited visibility into healthcare cost and outcomes data. Even when benefits teams are presented with all of the data, the disconnected legacy systems can prevent them from being able to understand what’s really working for their employee populations and what isn’t. Without a transparent, connected view of plan performance, it’s difficult for employers to justify investing in new digital solutions or determine how to innovate on current strategies so they can better meet the needs of their employees. Transparency into the overall healthcare quality and cost of the population is critical to make effective decisions, while still preserving the need to maintain privacy and security for individuals’ data.
How we can help:
At Collective Health, we launched a series of claims analytics tools that allow benefits leaders to clearly evaluate their benefits strategies by using service deep dives to contextualize claims data. These deep dives bring more detailed insights by service category (inpatient, outpatient, and more), clear visualizations, year-over-year comparisons, and enhanced filtering capabilities, without compromising the privacy of employees. We also calculate the cost and quality of point solutions, and provide this data against performance metrics from healthcare providers to identify whether and to what degree these point solutions provide return on investment. This way, we can provide a more holistic view of health plans while protecting employees. Read more here.
3) The Human Factor
Unlike other industries, the human element of healthcare can’t be completely replaced by technology. Healthcare systems were modeled with a mindset that most people would interact with the system once or twice a year, at a single hospital or in a clinical setting, to receive their necessary prescription or treatment. That model isn’t working anymore. With the rise in the population of people with chronic and complex chronic conditions (around 45% of the U.S. population), it’s clear that the healthcare needs of many people occur outside of their hospital or doctor’s office, and are ongoing. This high-touch, often-virtual, more frequent level of care requires personalized attention that several digital transactions could never replace. While technology can’t completely replace the human element of support for those with chronic conditions, it can and should be used to enhance it.
How we can help:
At Collective Health, we believe the human factor of healthcare is critical to a quality, personalized care experience, which is why we offer access to Member Advocates and a specialized service with our Care Navigation team. Member Advocates are our health benefits experts, who help all Collective Health members find solutions to issues and provide personal support in navigating today’s confusing and cumbersome healthcare system. Our Care Navigation team gives eligible members access to our team of nurses, pharmacists, social workers, and dietitians, providing clinical guidance and support for complex care needs.
This human interaction is then only enhanced by technology to further personalize the healthcare experience via Personalized Recommendations. Our Personalized Recommendations feature uses medical claims data to trigger a range of alerts, like helping to schedule a forgotten mammogram. These alerts, via in-app messages, email notifications and sometimes direct outreach from a Member Advocate, ultimately help members more easily navigate and understand their care. Read more here.
Interested in seeing how Collective Health’s products and services can help you drive more impact for your team, organization, and people? Fill out this form and we’ll be in touch!