At Collective Health we’re using advanced analytics, machine learning, and AI to solve some of the most interesting issues in healthcare and health benefits. We’ve found that sometimes problems and solutions lie in unexpected places.
Exploring Maternity Data
Recently, we dove into one of the topics our clients care most about—maternity.
For our clients, maternity was the #1 driver of healthcare costs in 2016. It’s also one of the biggest sources of member confusion. According to a recent survey of American adults conducted by Harris Poll on behalf of Collective Health, 70 percent of parents said they were confused about their healthcare benefits compared to 57 percent of participants without a child.
Specifically, our Data Science team wanted to see if CH Cortex, our patent-pending analytics engine, could identify any issues that our traditional reporting and metrics hadn’t yet picked up on. To do so, we considered all the interesting maternity data we have access to: claims information, benefit design details, utilization of our web and mobile products, engagement with our program partners, and the anonymized notes and inquiry data from when a member calls into our Member Advocates. Ultimately, we decided to run an initial unsupervised learning exercise with our member inquiry data, using 70,000 total words from 800+ maternity-related calls in 2016.
What’s unsupervised learning? It’s a machine learning approach where a system tries to find connections within unstructured data, like notes from a conversation. Basically, it’s using analytics to make order out of chaos, even if you don’t know exactly what type of order you’re looking for.
Surprising Findings
So what did CH Cortex reveal? Check out this word cloud below—it shows how often certain topics were coming up in member inquiries, with bigger words and word pairs indicating more frequent mentions.
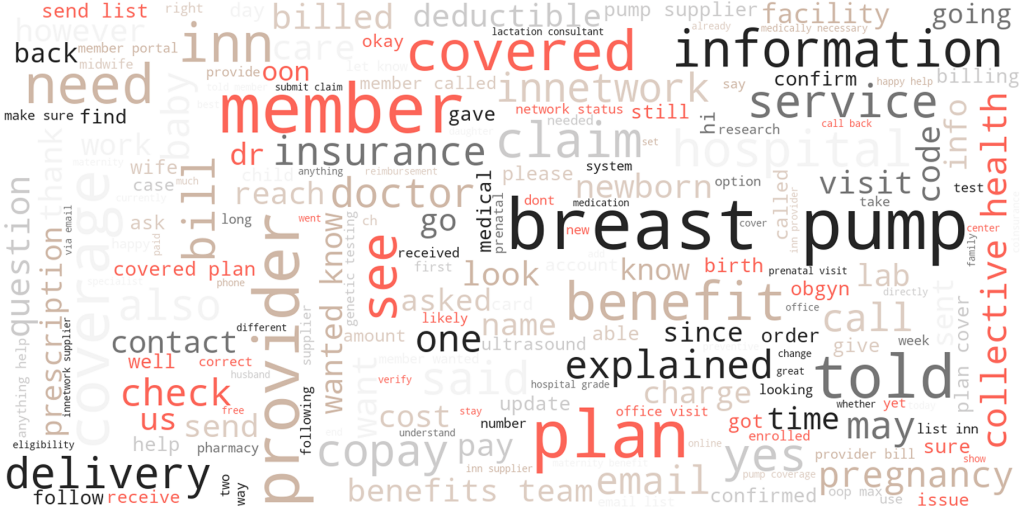
We were surprised to see how often one specific phrase kept popping up: breast pumps.
That piqued our interest, so we decided to dig a little deeper.
Next, we used a natural language processing model known as word2vec to learn vector representations for every word used in our Member Advocate notes. To understand some of the complexity in these word relationships, we used principal components analysis for visualization. That allowed us to cluster different words that were coming up in relationship to each other. When words appeared closer together it indicated that they were coming up together across lots of different conversations.
We found that words tended to group into two interesting clusters. First, there was a general questions cluster—members calling in with a set of common questions across coverage rules, in-network providers, and benefit design. However, there was also a very separate cluster—members just calling in with questions about breast pump benefits.
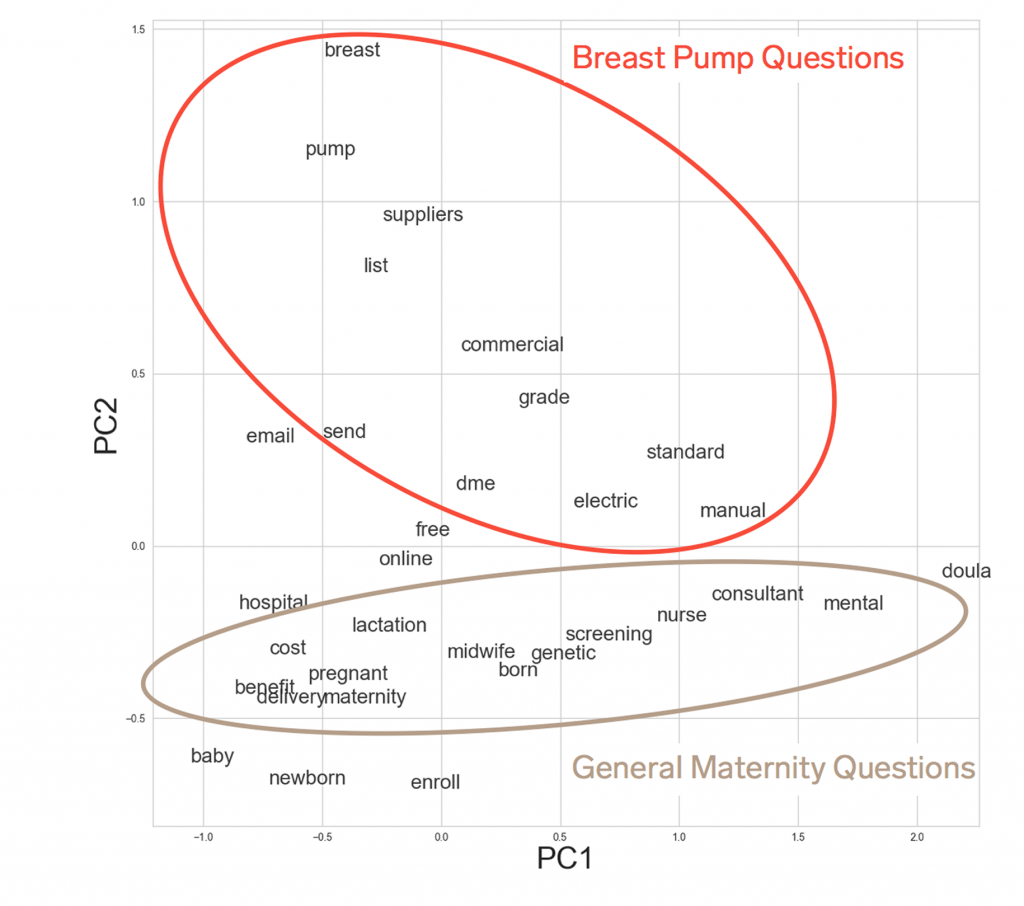
One of the great things about advanced analytics and unsupervised learning is that you can find things that you may never have known to look for. But, once you find them, they make immediate sense. The confusion around breast pump coverage is a perfect example of this.
The Truth About Breast Pumps
For most expecting parents, there are a lot of things to figure out as the due date approaches. Is the hospital bag packed? Have all the forms for parental leave been filled out? Do you have a birth plan in place? Is the paint in the nursery dry? Do you have diapers? Often it’s not until the last minute that the parents’ attention turns to the breast pump.
At that point, parents are confronted by mass confusion. What different kinds of breast pumps exist? Are they covered by insurance? What on earth is “durable medical equipment”? How do you get approval to purchase a pump? Who is an approved vendor? Why do I have to fax in forms? How long does it take to actually receive your pump? Will it get here in time?
Too often, with the due date looming, parents throw up their hands in frustration and switch to the back-up plan—they just go to a local store and buy a breast pump with their own money. This is especially frustrating because for the vast majority of our members, breast pumps are a fully covered benefit if you know how the process works.
This is a great example of healthcare complexity making it really hard for members to fully benefit from their health coverage. And it’s an example we may not have fully appreciated if CH Cortex hadn’t quantified the importance of it.
How We’re Simplifying Coverage
At Collective Health we’re lucky. Not only do we have great analytical tools, we also have many different member touch points through which we can directly improve the member experience.
Here’s what we’re doing to address breast pump coverage challenges:
- Member Advocate training: We built out even more breast pump resources for our Member Advocates so that when members call in with questions, we can quickly explain how their coverage works and help them clearly navigate the process.
- Member facing resources: We’re piloting a helpful digital Maternity Coverage Guide that members can use to self-navigate all the coverage issues associated with growing your family–from understanding your core coverage rules, to explaining how to procure a breast pump, to how and when to sign a newborn up for coverage. This Maternity Coverage Guide has become a great resource for our expecting parents and is already starting to preempt member questions and confusion.
- Simplifying explanations and coverage: Finally, we’re re-evaluating the way we talk about breast pumps in all of our web and mobile products. We’ve realized that a little more information and proactive guidance earlier in the maternity experience saves a lot of frustration and confusion at the end. We’re also re-evaluating the actual coverage rules and processes around breast pumps.
And we’re not done.
This exercise inspired an interesting question for us: If members don’t understand something as core as breast pump coverage, what else don’t they understand? What other assumptions have we, as an industry, been making about what members do and do not understand?
To begin to combat this confusion, we want to call out some of the most common questions our members have asked about their maternity coverage. Chances are, if our members have these questions, your employees do too. Do you have clear answers easily available? If not, sharing this information with your team might be a great first step.
- When do I need to enroll my little one so they are covered by my insurance?
Under most health plans, you have 30 days from delivery to enroll your baby for health benefits. Your HR team should be able to help you understand the specific details of your plan and add/enroll your baby. - My HR team told me I had a Qualifying Life Event. What does that mean?
Usually, you can only switch insurance plans once a year during Open Enrollment. A Qualifying Life Event, or a QLE as we say in the industry, is a time when something has changed in your life—like getting married, or having a baby—outside of the Open Enrollment period, and that change allows you the option to switch your insurance plan. Again, your HR team will have all the details. - What expenses can I use a DCA for?
Some employers offer a DCA—that’s a Dependent Care Account – alongside their medical benefits. If yours does, you can contribute funds, pre-tax, to use on qualified non-medical services for your new dependent’s care.
Stay tuned for more analytical insights from Collective Health. We have access to incredibly interesting data and are building uniquely powerful tools—and we’re just warming up.