What to do when a few members make up a large proportion of your company’s healthcare spending? Smart employers are choosing healthcare navigation programs to tackle the problem at the source by helping members make sense of their care, understand their treatment, and find resources to support them.
High-cost claimants (HCCs) are plan members whose healthcare claims take up a significantly larger portion of the financial resources than other members (as much as 31% of the total annual spend by an employer).
The disproportionate amount of patient care for these members can typically be attributed to traumatic events, serious illnesses, or chronic conditions and this imbalance can lead to a commensurate impact on the company’s bottom line.
However, with dedicated support from a healthcare navigation team, self-funded employers can rely on predictive models and data-driven algorithms to provide better care to every member.
Additionally healthcare navigation support can drive member engagement, improve patient advocacy for reductions and more, and enhance care coordination and utilization management—ultimately saving employers money while empowering their people.
The limitations with traditional care models
Traditional care management models have struggled to engage members and produce measurable value for employers. Historically, the industry has observed the following challenges to standard approaches:
- Members may be identified too late, or not at all.
- Standard cold outreach approaches to members tend to have low engagement rates.
- Most programs offer healthcare navigation by RNs, but lack a holistic approach.
What do healthcare navigators do?
At its essence, healthcare navigation refers to a service that helps companies from national brands to small businesses and their employees navigate the healthcare system, the enrollment process, their benefits packages, and ongoing care.
A healthcare navigator is a must in a patient-centric health system, as quality care must look at clinical care as well as lifestyle factors and mental health. Care navigators focus on improving health outcomes using cost-saving care coordination for policyholders from the social, geographic, and economic determinants of health as well as the clinical ones.
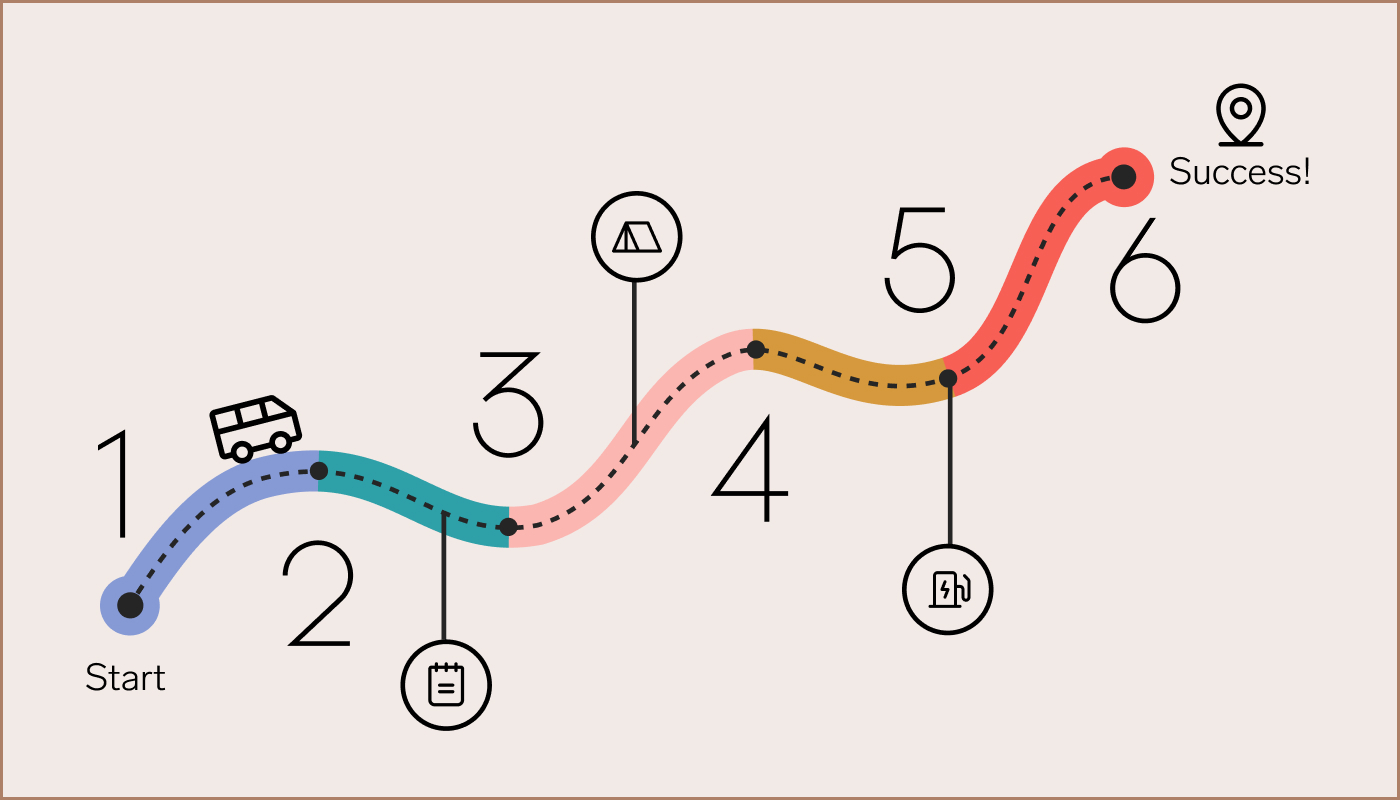
 Healthcare Navigation member journey with Collective Health
Healthcare Navigation member journey with Collective HealthAt Collective Health, our Care Navigation team can be trusted to review the health benefits and coverage options associated with a policyholder’s health plan, as well as critical provider data including claims, prior authorization, eligibility, engagement, and utilization to consistently find ways to streamline healthcare costs while improving and personalizing the patient experience.
Care navigation by Collective Health
Care Navigation’s philosophy is grounded in the principle of meeting members where they are, while empowering them with information and guidance that will impact them years down the line.
Early interventions and self-referral
Who knows better than the member that a health situation feels overwhelming and uncontrolled? This is why we accept self-referrals from members, whether or not they meet certain criteria or have progressed to the severity of being identified for outreach by our care managers.
Early intervention can often change the course of how a member experiences a healthcare event. Everyone’s threshold and rating of “health” is different and we’re here to support members with goals that support them in living the healthiest lives possible.
Focus on prevention, not just treatment
An ounce of prevention is worth a pound of cure. We believe a successful care management program should focus just as much on prevention as it does on treatment. This is why we don’t just assist people with managing chronic and acute conditions they already have.
We also ensure, with every assessment, that members have positive primary care relationships, are up to date on vaccinations, receive regular screenings to detect diseases before they become catastrophic, and are using necessary foundational health promotion services available to them.
Health challenges are multidimensional
Chronic health conditions do not exist in a vacuum. Programs targeting a specific disease can leave a member feeling just that, “targeted” for that condition, but any needs outside that disease remain deprioritized, even if they feel more important to the member.
By making our program disease-agnostic, we can prioritize what’s feeling most important to the member, knowing that a person can’t manage their diabetes well if depression is making it impossible to care about the number on the glucometer.
Reasons to implement health navigation
Healthcare should be personal and interactions with providers and insurers should be personable. With navigation services, it’s possible! Navigators improve the quality of care while ensuring lower costs for healthcare organizations.
The Collective Health member ecosystem allows easy care management for patients such as viewing and scheduling referrals or being reminded of routine appointments such as a mammogram or colonoscopy while also delivering the warmer outreach and follow-up required for a new cancer diagnosis.
Interdisciplinary experts on healthcare navigation teams
Our healthcare navigators include clinical specialists (nurses, pharmacists, and dieticians), as well as non-clinicians, such as social workers and care coordinators, who are familiar with diagnoses, treatments, plan details, and other resources, serving as access points to the system as a whole. Here are some of the unique elements of our clinical programs:
- We are able to better identify members through more holistic data analytics (claims, engagement data, etc.) and proprietary risk modeling.
- We build the trust members have in Collective Health in order to drive higher engagement.
- We intervene an interdisciplinary care team who are better equipped to support members with the issues that are top-of-mind (e.g., pharmacy, care coordination, and psychosocial support).
Healthcare navigation interventions
When your Collective Health plan goes live, healthcare navigation ensures that patients can locate and access appropriate treatments and resources, understand their conditions, and make informed decisions about their care plans.
Successful healthcare navigation works to alleviate patients’ physical, geographical, and emotional struggles and adequately address their financial needs. From coverage assistance to medication management, an enhanced patient-centric approach using healthcare navigators can help avoid the unplanned and high-cost emergency interventions that result from system inefficiencies.
Prescription drug optimization
This includes low-cost similar, retail-to-mail order conversion, conversion to preferred formulary drug, conversion from 30- to 90-day supply, and brand-to-generic conversion.
Site of care charges
This includes hospital to freestanding outpatient radiology, urgent care referral for frequent emergency room utilizers, and conversion to drug infusions from hospital/clinic to home.
Coverage assistance and optimization
This includes adjustment and resubmission of rejected prior authorizations, conversion from medical to pharmacy benefits to reduce member and/or plan sponsor costs.
Gaps in care closure
This includes missed vaccinations, mammograms, colonoscopies, and preventative care.
Medication management
This includes education on chronic conditions, correct drug usage, and high-risk medication review (e.g., chronic opioid use).
Learn about healthcare navigation today
Collective Health’s dynamic care navigation capabilities cover a broad range of patient needs and support good relationships and high engagement rates with policyholders. If you would like to learn how Collective Health’s healthcare navigations services can improve care and your bottom line, please contact us today.