By Dr. Sanjay Basu, Director of Research and Population Health
As our healthcare system tries to recover from the disruption caused by COVID-19, primary care practices across the country have been decimated. Make no mistake, this is a crisis within a crisis, as primary care has proven to be one of the most important institutions underpinning our healthcare and public health systems.
A quick primer on the importance of primary care, and its deterioration in recent years:
- Primary care is linked to improved life expectancy. In our research published in JAMA Internal Medicine, we found that every 10 additional primary care physicians per 100 000 population was associated with a 51.5-day increase in life expectancy, whereas an increase in 10 specialist physicians per 100 000 population corresponded to a 19.2-day increase.
- Availability of primary care has already been declining. We found that from 2005 to 2015, the density of primary care physicians decreased from 46.6 to 41.4 per 100 000 population. Primary care physician supply declined more in rural than in urban counties on average (–7.0 per 100 000 population vs –2.6 per 100 000 population). Concurrently, the number of specialist physicians increased from 699 989 in 2005 to 805 277 in 2015, corresponding to 68.0 per 100 000 population in 2005 to 71.3 per 100 000 population in 2015.
My colleagues and I from Harvard Medical School published a new paper in Health Affairs, a peer-reviewed journal, exploring the financial ramifications on primary care across the country as a result of COVID-19. The current pandemic has forced virtually all in-person outpatient visits to be cancelled in many parts of the country between February and May 2020.
As shown by the Commonwealth Foundation, only a subset of these visits were successfully replaced by telemedicine visits, many patients deferred necessary visits for chronic illness treatment and labs, and many needs of patients (such as in-person procedures) could not be replaced by telemedicine. We sought to estimate the potential impact of COVID-19 on operating expenses and revenues of primary care practices, to understand how COVID-19 might impact the availability of primary care for our members.
At a glance, here’s what we discovered:
- On average, a full-time primary care physician in the U.S. will lose more than $65,000 in revenue in 2020.
- Overall, the U.S. primary care sector will lose nearly $15 billion.
- Losses stem from drastic reductions in office visits and fees for services during COVID-19 shutdowns from March to May.
- Losses threaten practice viability, reducing further an already insufficient number of primary care providers in the United States.
These findings underscore the need for a plan that provides support for independent primary care doctors, including small independent practices, which tend to serve disproportionately rural and underserved populations.
We need a widespread, coordinated effort to prop up the primary care practices that are so critical to our communities. The paper itself proposes some efforts, including moving to capitation payments (such as paying practices per patient rather than per visit, to focus on caring for the population rather than just visiting patients more), and value-based payments (paying for keeping patients healthy, not just doing more labs or procedures). Recently, Blue Cross of North Carolina announced an important initiative to extend capitation payments and value-based payments, a step in the right direction.
Collective Health’s Approach
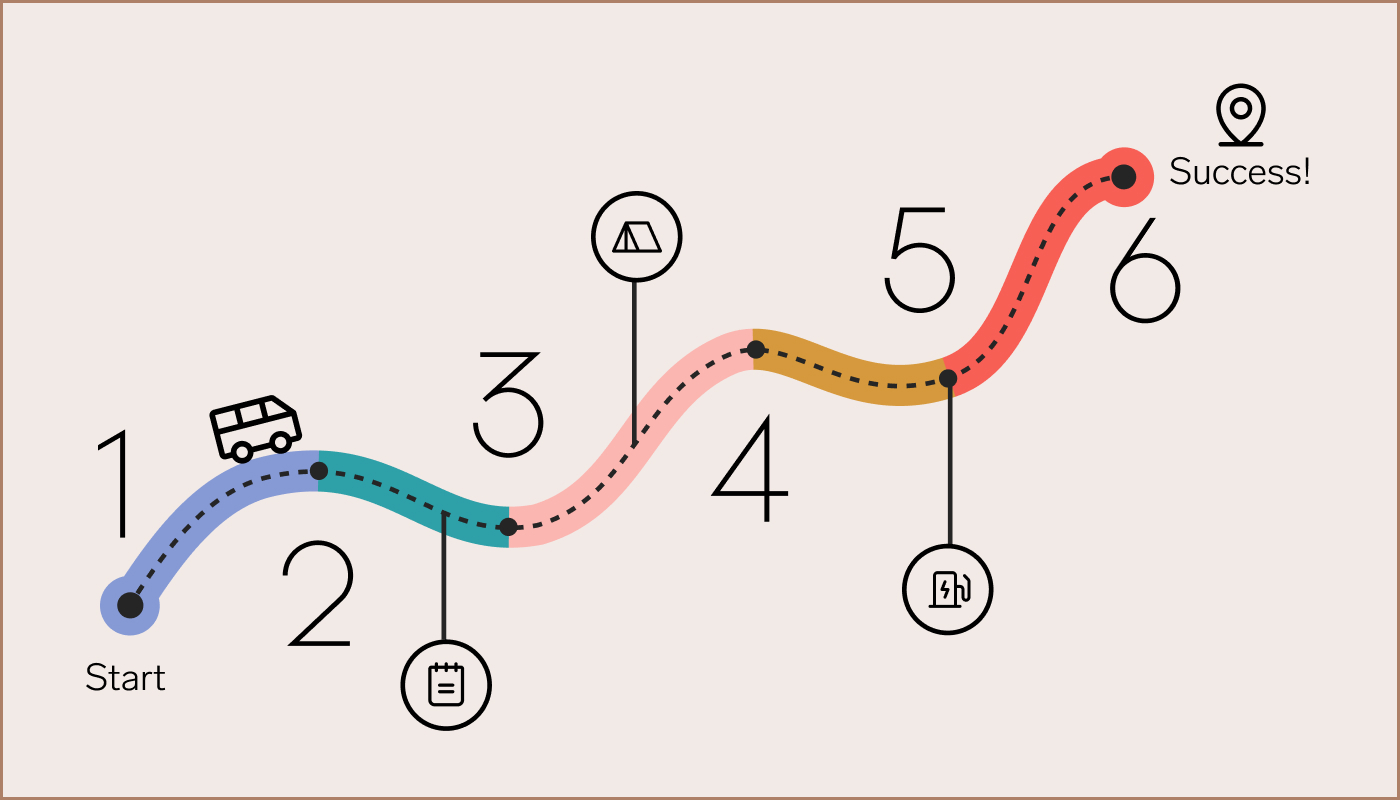
At Collective Health, we’ve invested in many such initiatives, and will continue to build on them. In the months to come, we’ll have more to share, including some early results. For now, here’s a snapshot of what we’re working on in an effort to support primary care practices across the country:
- A value-based insurance plan, based on extensive research conducted at the University of Michigan, that helps reduce barriers to accessing primary care and incentivizes members to engage in preventive healthcare and avoid low-quality healthcare services such as inferior surgical procedures or diagnostic tests that have been replaced by higher-quality and lower-cost alternatives
- Personalized communications from social workers, pharmacists, and nurses that help steer people towards primary care and urgent care instead of the emergency room when possible— both to ensure better prevention and continuity of care, as well as to reduce surprise medical bills and the risks of infection or other adverse events associated with emergency room visits. We’re working to build out additional personalized, digital guidance aimed at reinforcing navigation to more appropriate sites of care based on a member’s claims experience.
- Healthcare quality metrics and dashboards that keep track of gaps in care, such as missed cancer screenings, that enable proactive outreach to our members to remind them to schedule an appointment. We specifically focus on the Health Effectiveness Data Information System (HEDIS) measures maintained by the National Center for Quality Assurance, and a series of low-value care measures independently assessed by academic collaborators that help identify inferior medical practices.
- Independent assessments of third-party point solutions. Many services aim to augment primary care by providing digital touchpoints, such as digital linkage to glucometers for people with diabetes, or linkage to app-based behavioral health services or in-person fertility services. As per our recent JAMA Open Network study examining the effectiveness of near-site and on-site primary care services with One Medical, we can use our approach to provide an independent evaluation of point solutions.
For more information on Collective Health, please reach out.