By Dr. Ari Hoffman, Chief Clinical Officer | Collective Health
With hundreds of billions in lost productivity due to health-related problems, and billions spent on chronic diseases and unhealthy behaviors by employers every year, tackling the non-medical factors influencing your members’ health is critical.
The value shortfall of American healthcare is now so well established it is cliche: we pay too much for healthcare and fail to achieve better health as a society. Control healthcare spending per capita, or as a percentage of GDP, adjust for inflation, consider high level population metrics like life expectancy or dive into the nitty gritty of access and inequity… However you choose to slice and dice the data, the United States is a clear outlier on planet Earth when it comes to the value of our healthcare spending.
When it comes to spending on health, rather than healthcare, the US actually spends much of the money on downstream rescue care rather than the things that actually improve health. Add to that alarming findings on medical care avoidance during the pandemic due to COVID-19-related concerns (as many as 40% of Americans stayed away from doctors), it could be even more by the end of the year. If health is a state of physical and mental wellbeing, then what contributes to health?
Health-related work absences account for hundreds of billions of dollars per year in lost productivity
As little as 10% comes from healthcare, while the rest is determined by a mix of genetics, behavior, social and environmental factors. The social and physical environmental factors that provide a contextual backdrop to a human life are collectively referred to as social determinants of health (SDOH).
What are social determinants of health?
Health is a holistic concept that relies on more than just biological markers. It is, in part, determined by the environment in which we live as individuals. These non-medical factors play a significant role in health outcomes by influencing access to health care, nutritious foods, education, stable housing, etc. At its core, there are five social determinants of health:
- Healthcare quality and access, incl. health insurance coverage, the availability and quality of healthcare services in a given area, and the level of health literacy.
- Education access and quality, incl. level of education achieved, literacy, as well as early childhood education and development.
- Social and community context, incl. workplace conditions, discrimination, incarceration rates, community cohesion, and civic participation.
- Economic stability, incl. the financial resources available to individuals, income, cost of living, poverty, food security, and housing stability.
- Neighborhood and built environment, incl. housing quality, transport access, availability of nutritious foods, pollution levels, and neighborhood crime.
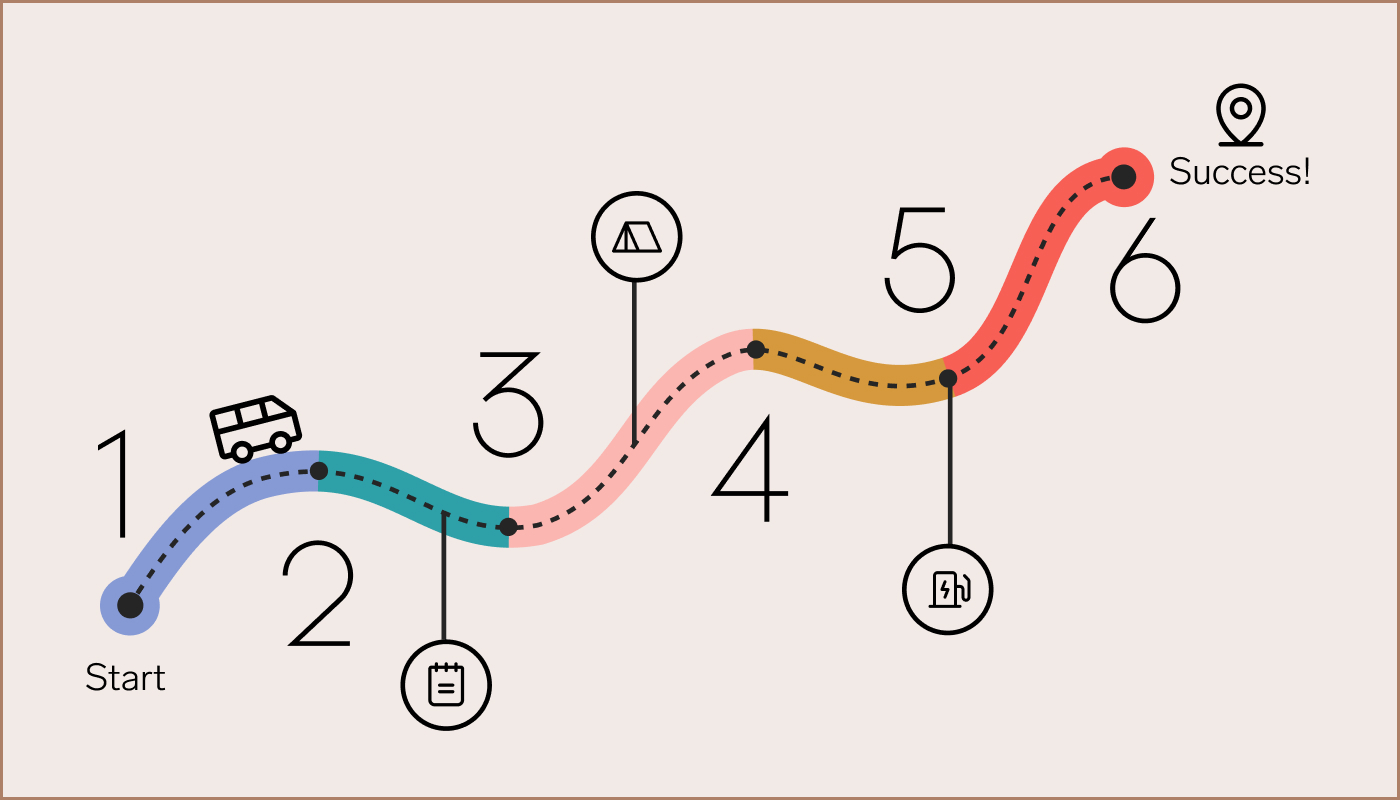
Employee populations, despite the rise of remote work, remain influenced by their locality and background, which also often informs the nature of their employment. Benefits leaders who understand these factors are empowered to deliver meaningful programs that engage employees by meeting them where they are on their health journey.
Download this free White Paper now
Social determinants at work
A central challenge in addressing SDOH is that the magnitude of the problem is so large that it feels outside the sphere of influence for both individuals and employers. Topics like economic inequality are overwhelming, and overwhelming can quickly lead to inaction.
Low wage workers face additional affordability and access challenges, driving disparities in healthcare utilization and costs.
Early in my career as a physician, I grasped the critical nature of SDOH but didn’t necessarily feel it was my responsibility to address these thorny problems, nor did I feel well equipped to do so. As my career progressed and I learned more, I recognized that we ignore the structures of people’s lives at great cost.
Take the example of a patient with high blood pressure who is prescribed a medication, but who is subsequently hospitalized with blood pressure so high it pinches off the blood flow to vital organs. The myopic view that focuses solely on healthcare leads to the conclusion that the medication was underdosed, or the patient needs two blood pressure medications.
Only when we zoom out and see the context of that patient’s life do we discover that the medication was unaffordable and the assigned pharmacy inconvenient. Transportation and affordability are the problem, not the medication itself. The same is true for employers given the outsize role that SDOH play in the health and wellbeing of the workforce.
Read it now on the blog
Social determinants affect employers and productivity
Employees don’t leave SDOH at the door, they bring them to work every day. For companies, this can result in both absenteeism (missing work due to poor health) and presenteeism (decrease in performance and productivity at work due to poor health), not to mention workforce-wide effects on productivity, satisfaction, and general wellbeing. All of this amounts to hundreds of billions of dollars per year in lost productivity from health-related work absences, not even counting medical and pharmaceutical costs.
Consider this. A retail worker diagnosed with diabetes type 2 lives in a marginalized neighborhood with poor transport links. Without access to or the ability to obtain private transport, attending work is a challenge in itself, let alone making it to medical appointments to monitor and manage diabetes. These challenges, which have nothing to do with medical status or cost, present significant obstacles to obtaining care and managing their health. As a result, this patient is more likely to experience further health decline and rising medical costs.
 The cost of poor health has serious ramifications for employers
The cost of poor health has serious ramifications for employersThe burden of social determinants is not equally shouldered across the population, and the same inequities will apply across the workforce. Some of this disparity will be geographic, with unique access challenges in rural America, environmental health impacts of industrial or mining regions, or food deserts in more impoverished areas.
Other disparities will be seen by race, language barriers, age, and level of education, to name a few. Low wage workers face additional affordability and access challenges, driving disparities in healthcare utilization and costs. Some disparities are condition-specific. Cancer patients are particularly vulnerable due to the high costs of modern cancer care. One study showed that 42% of cancer patients depleted their entire life savings in the first two-years after diagnosis.
This leaves employers with a lot to consider, especially with remote work and increasing geographic spread of employees. For example, a large retailer may have a segment of workers at headquarters, another at distribution centers, and a third in stores, crossing many wage strata and spanning rural to urban. Some employers have regional populations, while others have employees across the globe. Working with partners to administer benefits and help members navigate care, employers and their benefits partners can use these insights to target resources where they are needed most.
Tackling SDOH in your employee population
It’s an intimidating thought, trying to unravel and understand the societal forces at work within your employee population, but making that decision has the power to transform your approach to employer benefits and empower your employees, not just at work, but in the home too.
It takes work to know your employees this well, to hear their stories, to meet them where they are. However, the benefits (pardon the pun) far outweigh the risks associated with overlooking the social determinants of health. From increased productivity and better cost control to staff retention and greater quality of life, HR leaders on the front lines of the talent wars are learning to adapt by customizing their programs to the needs of their workforces. And you just might find that the empathic listening required is therapeutic for all involved.
From a clinical perspective, I see the innovation in digital health and virtual care driven by the pandemic as a means to match interventions with people’s individual needs, deliver the care that they need when and where they need it, and empower them to live healthier and happier lives. As these new technologies develop and evolve, they will likely bear fruit for employer benefits programs too, helping America’s largest providers of health coverage to build a better world starting in their front yard.
Read it now on the blog