Better employee healthcare at a lower cost is possible.
In fact, a recent independent, third-party study proved that better employee healthcare at a lower cost is not only possible, but the reality for the Collective Health customers they studied. The Collective Health Cost Impact Study, conducted by global professional services firm Aon, found that our integrated health benefits solution cut the cost trend of healthcare benefits for included employers by 50% over a five-year period.
Researchers compared the medical and pharmacy costs of two employer groups who have used Collective Health since 2017 to a matched control group. They also looked at how Collective Health members were using digital tools like My Collective™, plus real-time support from Member Advocates and the Care Navigation™ team, to engage with their health benefits.
Here are the key findings:
Collective Health members in the study had lower overall healthcare costs than their counterparts in the control group.
Although not part of the study, we estimate that in aggregate, the Collective Health solution helped those customers save approximately $11 million over the time period studied.
The study revealed that members who used Collective Health had high engagement with care advocacy and guidance, fewer trips to the emergency room, and increased use of preventative care. All of these factors likely drove meaningful savings for our customers when it came to healthcare costs.
The study based these findings on its Cost Efficiency Measurement (CEM) methodology, which precisely matches members using Collective Health to those in a control group according to geography, age, gender, and chronic conditions. This methodology minimized the impact of common challenges when measuring the outcomes of benefits programs (including the impact of network discounts and utilization changes due to the COVID-19 pandemic) and allowed researchers to identify the following results:
- The cost trend for studied Collective Health customers during the five-year period was 7.2%, less than half of the 14.9% increase seen in the control group.
- Collective Health customers in the study saw cost efficiencies compared to market control across all of the top 10 most prevalent condition groups analyzed. Members with diabetes, hypertension, musculoskeletal conditions, and behavioral health diagnoses saw the greatest improvement in cost efficiency over time.
- The claims cost for members with two chronic conditions during the study period had a statistically significant improvement from $57 per member per year above control in year one to $1,130 below control by year five.
- Collective Health customers in the study reduced claims spend on outpatient surgery, radiology, and advanced radiology (CT, MRI, PET) during the study period when compared to a control.
Members on the Collective Health platform engaged with their benefits at high rates and engagement increased with clinical complexity.
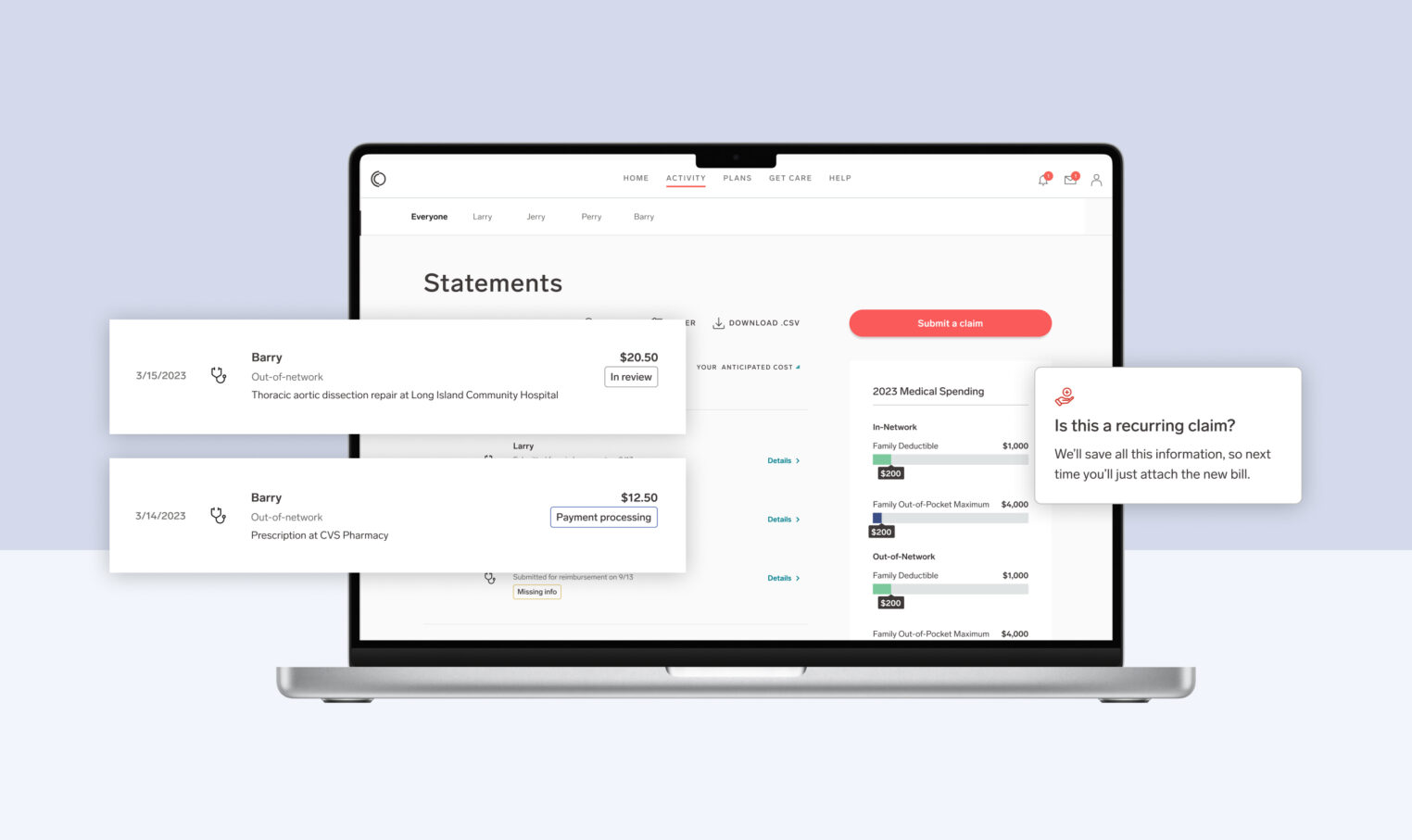
Our mission at Collective Health has always been centered around improving the member experience. Our My Collective™ platform is designed to give members everything they need to engage in their healthcare journey, from medical, dental, vision and pharmacy, to supplemental benefits and point solutions, all in one place.
The Collective Health Cost Impact study measured engagement in three ways: Member Advocate inquiries, participation in our Care Navigation program, and digital engagement, which occurs when a member logs into the My Collective™ app or web experience.
Here are the key findings from the comparison of studied Collective Health members to industry benchmarks:
- Collective Health members had high engagement, which increased for members with increasing numbers of chronic conditions.
- Eligible members with two chronic conditions improved to be significantly below market level.
- The increased engagement rate among Collective Health members with complex conditions is correlated with higher cost efficiency improvement over time.
Download the full Collective Health Cost Impact Study today to learn more about these compelling findings.