Picture this: you’re traveling outside the country on an exotic vacation (exciting!) when you catch a stomach bug (bummer). You visit a doctor in the area for care and head home from your trip, feeling better. That memory, however, isn’t just for your travel journal. The care you received was out-of-network, and that requires submitting a claim for reimbursement.
Out-of-network submission claims can result not just from an unexpected illness outside the country, but any healthcare visit that involves an out-of-network doctor. It could be for institutional care needed but not offered within an approved network, medical equipment, or travel expenses incurred when receiving care not found locally.
Submitting out-of-network claims can sometimes feel confusing, and at Collective Health, we want to simplify the process. We’ve listened to member feedback and have released some updates to our claims submission process that we think you’re going to exclaim with joy about! (Exclaim, get it? Ok, we’ll see ourselves out now.)
Track your claim status in real time
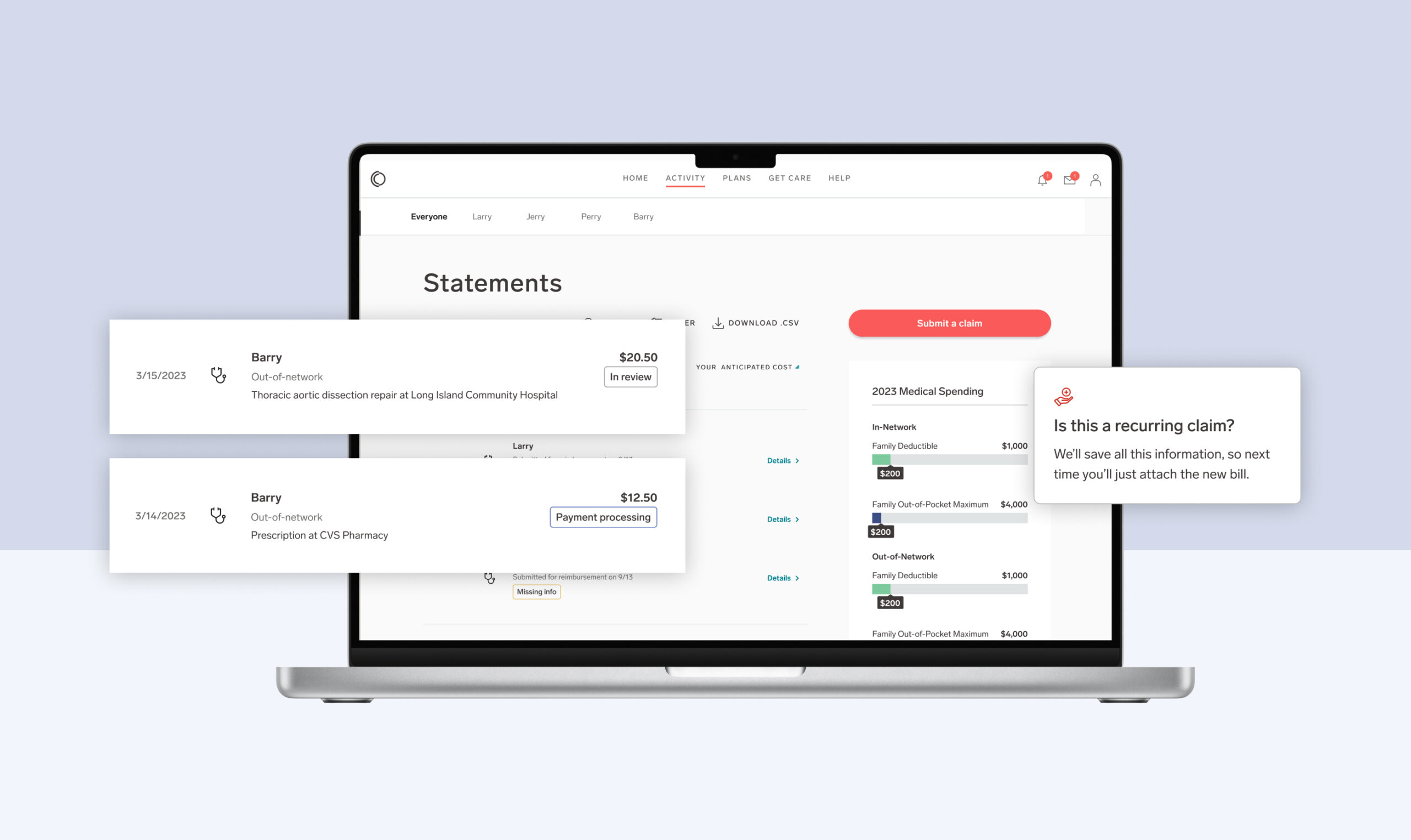
If you’ve ever submitted an out-of-network claim and wondered what the status is—wonder no more. When you submit your claim through My Collective™, you’ll see a list of claims in progress on the Activity page. This is meant to keep you informed as Collective Health works with your health benefits plan to process those claims. There will now appear one of three statuses next to your claim:
- Received (this means we’ve got it)
- In review (this means we’re working on it)
- Missing info (this means there’s something that we need before we can complete the processing of this claim. If you click on the details of the claim, you’ll be taken to your inbox where there will be a message explaining what you need and how to get it so we can get your claim processed.)
Once the claim is approved, you’ll see a payment tracking status added to the claim, with one of the following statuses: Payment approved, Payment processing, or Paid. You’ll now know exactly what the status of your claim submission is with these new updates.
Get your reimbursement–right to your bank account
Our updated payment registration process now has direct deposit, in addition to checks, as a payment option. You can now receive your payment faster and directly to the bank account of your choice.
Save recurring claims, automatically
If you’ve ever needed to submit a recurring claim, you know re-entering the same claim information on a weekly or monthly basis can be time-consuming and frustrating. Now, if you have a recurring claim, you can save the information to avoid adding it everytime, and it only requires an attached bill to complete entry.
The platform also automatically saves incomplete submissions for completion later. Claims can be started online and finished on the app (and vice versa). This allows you to save your work in-progress and complete your submission on your own time, on your own terms.
We hope that with these updates, submitting your out-of-network claims is a breeze! If you're looking for more information, check out the Help section within My Collective™.
And if you're a benefits leader, broker, or consultant looking to learn more about Collective Health, schedule a demo with our team.