Family-building benefits are a relatively new frontier for employers, which means they’re not always well understood. Our Premier Partner Carrot Fertility, a provider of fertility and family-forming benefits, explains the different care modalities and resources involved.
What comes to mind when you think of infertility? During Infertility Awareness Week and beyond, the conversation often focuses on cisgender women going through in vitro fertilization (IVF) after a diagnosis of medical infertility. IVF is a costly procedure that’s a critical option for many families. Most traditional health insurance plans don’t include coverage for IVF — and improving access is an impactful goal. But too often, the conversation around infertility support stops there. Why is this a problem?
For one, a medical diagnosis of infertility isn’t the only barrier to family forming for many. Medical infertility is defined as a different-sex couple trying to get pregnant without success for six to twelve months, depending on age. Many LGBTQ+ couples and single-intending parents don’t meet those criteria but still need additional support to grow their families.
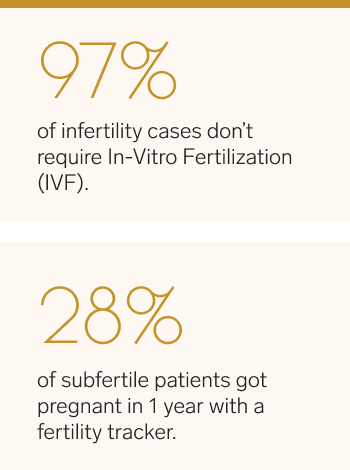
Only 3% of infertility cases need interventions like IVF.
IVF also isn’t the only treatment for infertility. One in eight different-sex couples are diagnosed with infertility, but fewer than 3% of infertility cases need advanced reproductive technologies like IVF. And infertility isn’t limited to cisgender women. In different-sex couples, about one-third of infertility cases can be traced to the partner with ovaries and one-third to the partner with testes.
For employers who want to provide robust resources for employees, it’s essential to understand all of the family-forming resources and options employees need access to, including first-line interventions, journeys like donor-assisted reproduction and adoption, and emotional support along the way.
Find out more
Starting the process: fertility testing
Several fertility journeys start with testing, whether someone has been trying to get pregnant, is considering fertility preservation, or wants to learn more about their family-forming options as an LGBTQ+ couple or single-intending parent.
At a fertility consultation, patients will typically discuss their family-forming goals and medical history, then take a blood test to measure hormone levels or semen analysis. These tests are usually done in a clinic, but at-home fertility testing is also an option.
How can employers help?
Traditional insurance typically only covers fertility testing for different-sex couples that have been trying to get pregnant for six to twelve months. Providing access to testing without this requirement helps your employees learn more about their health and take proactive steps earlier on.
First-line interventions: cycle tracking
We mentioned in the introduction to this post that only 3% of infertility cases need interventions like IVF. So what about the other 97% of infertility cases?
Sometimes, fertility assessments find certain problems that can be addressed through hormonal treatments, a simple procedure called intrauterine insemination (IUI), or surgery to correct a physical problem.
Interestingly, some people with a history of infertility can get pregnant without any treatment. One Australian study found that more than 40% of women aged 28–36 with a history of infertility ultimately got pregnant without treatment.
Cycle tracking is one way for couples to increase their odds of getting pregnant. Phone apps, a simple calendar, and wearable fertility trackers are the options available at this stage.
How can employers help?
Cycle tracking through apps and calendars is free, but employers can help employees who are pursuing this option by providing educational resources and higher-tech fertility tracking devices. One study found that a wearable fertility tracker helped 28% of subfertile users get pregnant within one year, potentially avoiding more invasive fertility treatments down the line.
First-line interventions: nutrition
Nutrition is another lesser-known intervention that can have a significant impact on fertility. Diets high in unsaturated fats, whole grains, vegetables, and fish have been associated with improved fertility in all genders.
On the other hand, saturated fats (like those found in red meat, butter, and cheese) and sugar have been associated with poorer fertility outcomes. One study found that folic acid (found in foods like leafy greens), vitamin B12 (found in foods like eggs), and omega-3 fatty acids (found in foods like fish) were all linked with positive effects on fertility.
How can employers help?
While nutritionists may not be the first experts that come to mind when you think of fertility professionals, they can play a valuable role in optimizing fertility outcomes. Look for fertility benefits that include access to a range of expert support, not just fertility clinics.
Taking the next step: donor-assisted reproduction
Donor-assisted reproduction is an essential option for LGBTQ+ couples, single-intending parents, and anyone who isn’t able to use their own gametes. Individuals and couples may use a sperm or egg bank or donor agency to find a donor or ask someone they know.
In sperm donation, a person who is not the intended parent provides sperm for fertility treatments such as intrauterine insemination (IUI) or IVF. Reasons for considering donor sperm may include:
- Same-sex, cisgender female couple or single-intending parent who is cisgender female
- Lack of sperm in semen (azoospermia) or problems with sperm quantity or quality
- Damage to the testes (e.g., from chemotherapy or radiation treatment)
- Ejaculatory dysfunction
- A genetic condition in the intended parent that may impact the health of the child
In egg donation, eggs are fertilized through in vitro fertilization (IVF), and the resulting embryo is transferred to a uterus. Reasons someone may consider using a donor egg include:
- Being on a gestational carrier journey
- Problems with egg quality or quantity (e.g., diminished ovarian reserve or early-onset menopause)
- Damage to the ovaries, such as during chemotherapy or radiation treatment
- Having been born without ovaries
- A history of unsuccessful IVF cycles using one’s own eggs
- Genetic disease
Gestational carrier journeys (surrogacy)
Gestational carrier (GC) services are also an option for those with conditions that make it impossible for someone to carry a pregnancy, such as cancer treatment. Same-sex couples may also choose GC services.
One common misconception about GC services is that a carrier, also known as a surrogate, uses their own eggs to get pregnant. This process is commonly now referred to as “traditional” surrogacy.
Today, most GC journeys also involve using an egg donor in a process known as “gestational” surrogacy. Gestational surrogacy involves fewer legal risks and is the preferred option for the majority of couples and individuals pursuing this path. The cost of a successful gestational carrier journey is more than $100,000.
How can employers help?
Donor-assisted reproduction and GC journeys involve several medical, legal, and logistical steps. For example, when using egg, sperm, or embryo donors or GC services, intended parents need an attorney to create contracts regarding the legal implications around parental rights and obligations.
If someone chooses to work with a known donor, the process can become even more complex. Inclusive fertility benefits should include access to agencies, sperm banks, and legal services and include care coordination for guidance around each step of these complex paths.
Taking the next step: adoption
There are many reasons that people may decide to adopt a child. For some, it’s how they prefer to become a parent. For others, the decision comes either during or after an infertility experience.
In the U.S., there are multiple paths for adoption, and each comes with a unique set of regulations and challenges. For instance, adopting between countries has very different requirements compared with domestic adoptions.
There’s also a difference between private adoption and adopting through foster care. Foster parents can serve as a temporary placement for a child until they return to their birth family, and if that can’t happen, they may adopt the child. For many families, the adoption process takes several months or even years.
How can employers help?
Adoption assistance programs through employers help reduce the financial burden of these journeys; domestic, private adoptions typically cost between $30,000 and $50,000, and intercountry adoptions can cost between $30,000 and $60,000.
Employer benefits can also help employees connect with the right adoption journey for them. It’s still legal in some states for adoption agencies to discriminate against same-sex couples on religious grounds, so having guidance is particularly valuable for LGBTQ+ prospective adoptive parents.
Ongoing support: mental health and fertility
One stressful part of many fertility journeys is the cost involved. As we’ve discussed, different family-forming journeys can also be logistically complex. And while it’s tough to tease out the ways in which mental health issues impact fertility and vice versa, experts do believe that psychological factors such as stress can increase the risk of infertility as well.
How can employers help?
Fertility benefits can help alleviate the financial and logistical stress associated with infertility and family-forming journeys. It’s also important to make sure employees have access to mental health professionals with experience working with those going through fertility and family-forming challenges. Feelings of isolation are also common in fertility journeys; ongoing support can help employees feel less alone.
Expanding the conversation
Part of the goal of the Infertility Awareness Week is to expand the conversation around infertility and show that it can impact a larger portion of your employee population than you might expect. By growing your understanding of the different paths to parenthood employees take, you can provide support that meets the needs of all of your employees, no matter which journey they pursue.
Learn more about how Carrot’s inclusive fertility benefits can support your employees.
Disclaimer: The views expressed in the article are those of third parties. They do not purport to reflect the opinions or views of Collective Health or its members.