Smart companies know. They know that you can’t overlook the health and well-being of employees and their families, and the brightest leaders today do more than simply react—they embrace what’s next. While health benefits have traditionally been a black box for employers—the largest sponsors of healthcare in America—there are now a variety of ways for companies to take better care of their people while maximizing every dollar spent.
Over the last few years, we’ve seen our self-insured employer clients—which include some of the most forward-thinking companies in the country—break further away from a status quo that has plagued health benefits for decades. This takes on many forms: from the adoption of new technologies to exploring innovative care solutions to breaking down unnecessary barriers to receiving treatment.
We recently took a deeper look at some of the latest trends in health benefits design across our book of business. If you’re a benefits or HR leader eager to build a benefits package that can improve your people’s wellbeing and bolster your recruiting and retention efforts, here are a few ideas.
1. Maternity and fertility benefits are critical. Make yours great.
Although parental benefits in the U.S. have traditionally lagged behind other countries, we’re seeing a shift among employers in providing their people with exceptional perks in this area. Several of our own clients are deploying world-class family benefits—Pinterest, for example, has a world-class parental benefits package. Here are a few suggestions:
- Push the limits of your self-funded plan to support the new parents on your team, as there are often solutions to complex issues in plain sight. For example, understanding how to pay and get reimbursed for a breast pump—a basic necessity for any new mother—is still a challenge in 2019. Helping simplify an unnecessarily complex process like this is key for your people. A policy we’ve established at Collective Health enables employers to provide out-of-network breast pumps at in-network cost sharing to make the process much more seamless. Currently, 87% of our clients have opted into this policy.
- Embrace the latest in innovation, and realize efficient use of your healthcare spend. Companies like Cleo have developed a variety of powerful employer solutions to guide families through the maternity process, from pre-pregnancy through parenthood and beyond. Companies like Progyny are taking advantage of advancements in medicine and new technologies to achieve superior clinical outcomes and ultimately make fertility treatment—from IVF to preimplantation genetic testing—more accessible. As of 2019, almost 1/3 of all health plans we administered offered a third party solution to enhance employee access to fertility treatment.
2. Health tech is everywhere. Cut through the noise to understand what programs are most important for your people.
According to Rock Health, 2018 was the biggest year for digital health funding to date, with $8.1 billion invested in health tech companies tackling a variety of issues from therapeutics to genetic testing. American employers have become an accelerant to healthcare innovation as companies across the country continue to put the latest health solutions to the test. Our clients are at the forefront of adopting digital health and evaluating its impact:

Third party solutions can fill gaps in your health plan, but it’s important to understand which will benefit your population most and to measure their effectiveness. A starting point is requiring your health plan administrator to provide claims data regularly to identify patterns in your population health—and if you have the resources, survey your people anonymously to get even more granular. From there, you can determine which programs might make the most sense, implement them, and begin collecting engagement data for each. Over time, you’ll want to assess the relationship between engagement with these services and the impact it’s having on employee satisfaction and/or claims.
3. New clinical solutions can supplement traditional health plan offerings.
As companies look for ways to help their employees access more efficient, high quality primary care, many are turning to on-site and near-site clinical programs being offered by companies like One Medical, Crossover Health, Heal, and more. These companies are delivering care with a focus on a premium user experience, and with the goal of encouraging employees to lean into their health now in order to prevent more serious issues down the line.
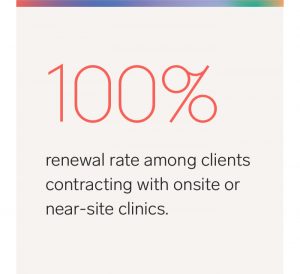
Our platform enables companies to easily implement new clinical offerings, and we’re seeing our employer clients increasingly take advantage of these programs because they are excited by the potential these solutions have to lower the total cost of care and improve employee health. This year, we saw a 100% renewal rate among clients contracting with onsite or near-site clinics.
Additionally, walk-in retail clinics have emerged as a convenient way for people to be treated for common health issues like a sinus cold or sore throat. Employers can leverage these facilities to save costs, and to provide quicker access to basic care for their people. As of 2019, 100% of our clients cover walk-in retail clinics as part of their health plans.
4. Write your own rules to provide better access to behavioral health treatment.
As a society, we’ve made strides in how we talk about and treat behavioral health. Unfortunately, systemic barriers to behavioral health treatment remain in place. Behavioral health continues to be an important public health issue (impacting roughly 1 in 5 adults), and many people don’t get the support they need.
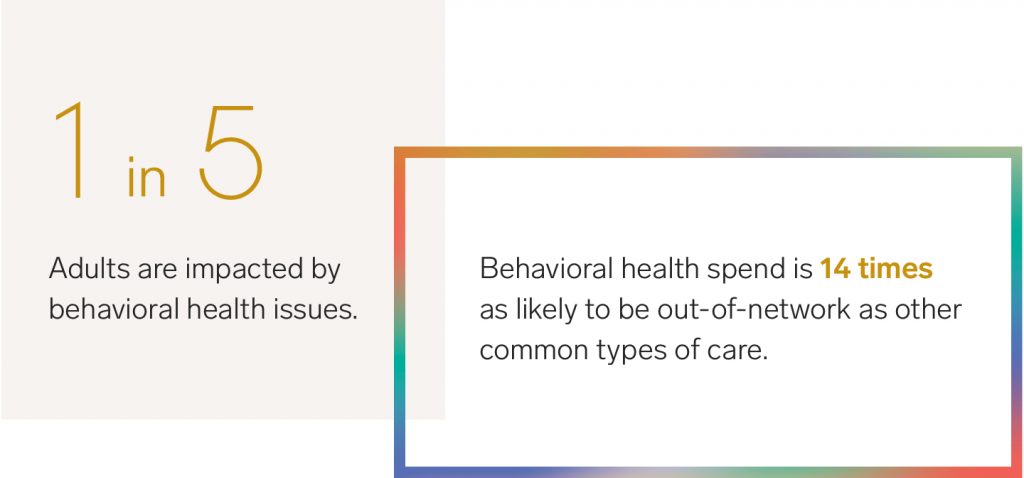
Why? For one, there is no shortage of demand, so there is often little incentive for providers to be in-network to attract patients. Secondly, many behavioral health services are often regarded as specialty treatment, forcing people to go out of network and pay higher out-of-pocket costs, or worse, avoid treatment altogether. For context, claims data from Collective Health shows that behavioral health spend is 14 times as likely to be out-of-network as other types of care like primary or preventative.
However, we’re seeing employers find new ways to help their people bypass these hurdles. This includes:
- Adding third party solutions like Lyra and Modern Health to expand access to care.
- Treating out-of-network behavioral health treatments as in-network, meaning employees pay the same amount for treatment regardless of who they visit.
- Covering out-of-network behavioral health services on their plan even if the plan doesn’t cover out-of-network services for other care areas.
- Setting a lower coinsurance amount for out-of-network behavioral health than for other out-of-network benefits.