We recently hosted our Care Navigation™ webinar where we sat down to discuss how our unique personalized, holistic approach to care management keeps the member at the center of everything, enabling better health outcomes for members and helping companies see healthier bottom lines.
You can watch the full webinar here.
Here are some of the most common questions around Care Navigation that we hear from brokers and employers.
What is Care Navigation?
At Collective Health, Care Navigation plays a crucial role in helping people get the right support, at the right time, across a wide range of complex health needs. Our Care Navigation program is a “complex” care management program. We aim to identify high-risk and rising-risk members early in their care journey, and help them navigate their medical and psychosocial needs.
Describe your staffing model.
Disjointed care can result in increased costs and a frustrating member experience. Providing the best holistic care management begins with the team. Our Care Navigation team is composed of Collective Health pharmacists, social workers, nurses, dieticians and Care Coordinators, and we continue to evolve the team based on the needs of our members.
How do you engage members? And how do you define engagement?
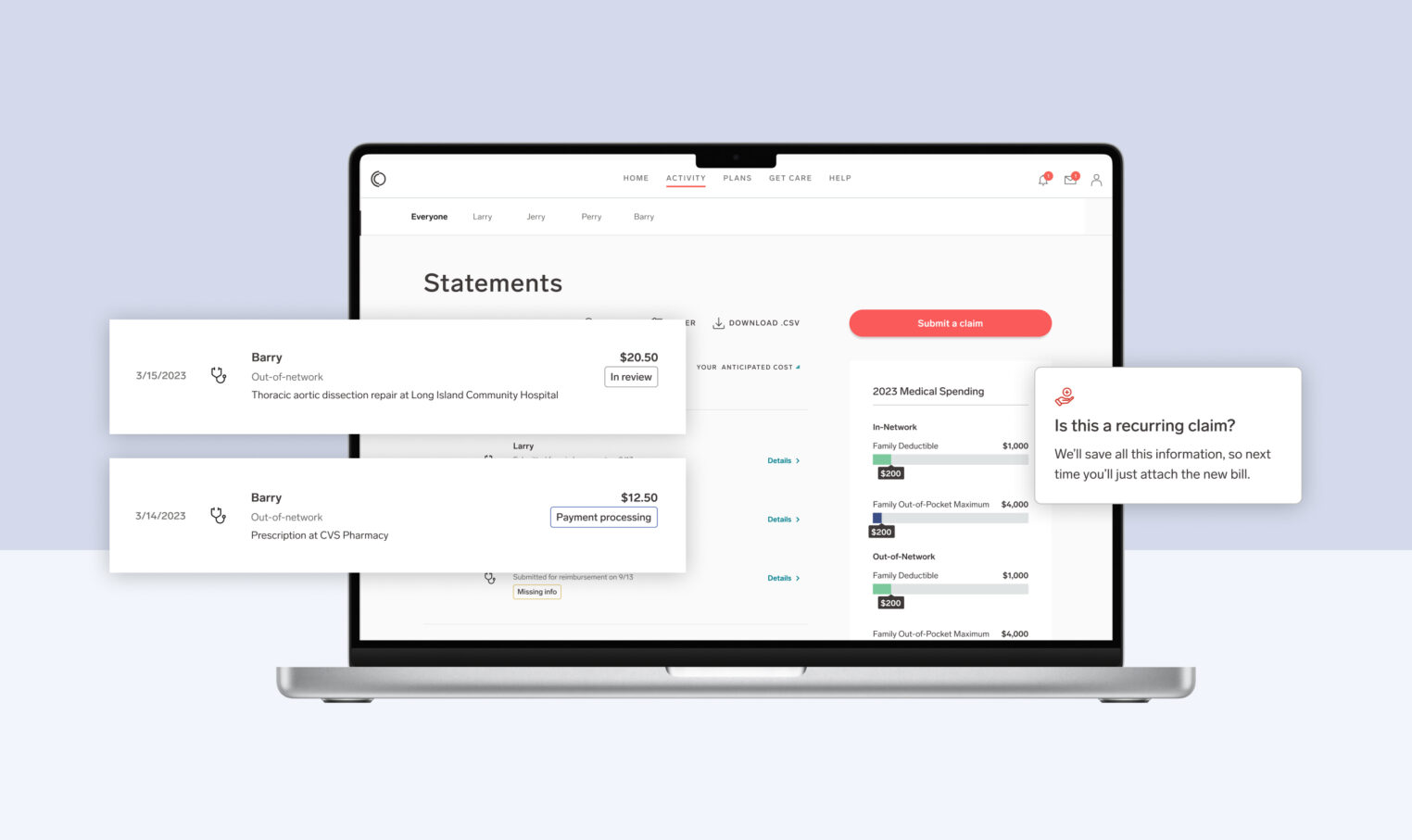
We leverage our role as an employer’s plan administrator and our access to real-time claims and engagement data to quickly identify members in need of support. We begin with a secure message to introduce ourselves, what we offer and how to get a hold of us. This is followed up with a phone call from a clinician. If we are unable to reach the member we leave a message then follow up with another email. We also allow for self-referrals so members may call us directly for care management services.
Once a member is engaged in care management a complete assessment of needs is completed including a depression screening and a social determinants of health screening. Members may engage with one or all of our care managers, depending on needs. This may be a social worker, registered nurse, pharmacist or dietician. Regardless of the resource, we engage members with empathy—focusing on listening to their needs above all. This approach leads to higher engagement rates compared to traditional carrier-led care management programs, and an exceptional member experience.
We engage 35% of complex care members. And we define engagement in a more stringent way than many other industry players. To us, engagement doesn’t mean that we just leave a voicemail or quickly catch someone on the phone before they hang up. In order to be included in this data set, we require that the member has agreed to be in care management, and have one goal set, which means they also have a follow up scheduled.
How do you impact the total cost of care?
Collective Health influences total cost of care by providing clients with a menu of options on how they’d like to organize plans, including which levers to pull in terms of personalized engagements for members. For example, clients can pull levers related to the site of service for imaging, orthopedic surgery and other elective surgeries in order to help steer members to certain high value, lower cost opportunities. We also influence total cost of care through our holistic approach to care management which can include services like our pharmacist interventions, which have led to savings of $10.38 per employee per month (PEPM), or an ROI of 2:1 across the entire program.
How does your care management approach differ from the other solutions in the market?
Unlike other solutions in the market, we believe complex health issues are often a result of socioeconomic factors, and it’s why we put an emphasis on social determinants of health—for example, how members’ geographic location impacts their access to food or transportation—as part of Care Navigation. We also are a disease agnostic care management program, which means we manage any disease process, rather than picking the top 5 or the most common. We also don’t require a certain cost threshold prior to a member being able to enter into care management. We believe that intervening early and effectively is the greatest opportunity to impact costs and to serve our members in a meaningful way.
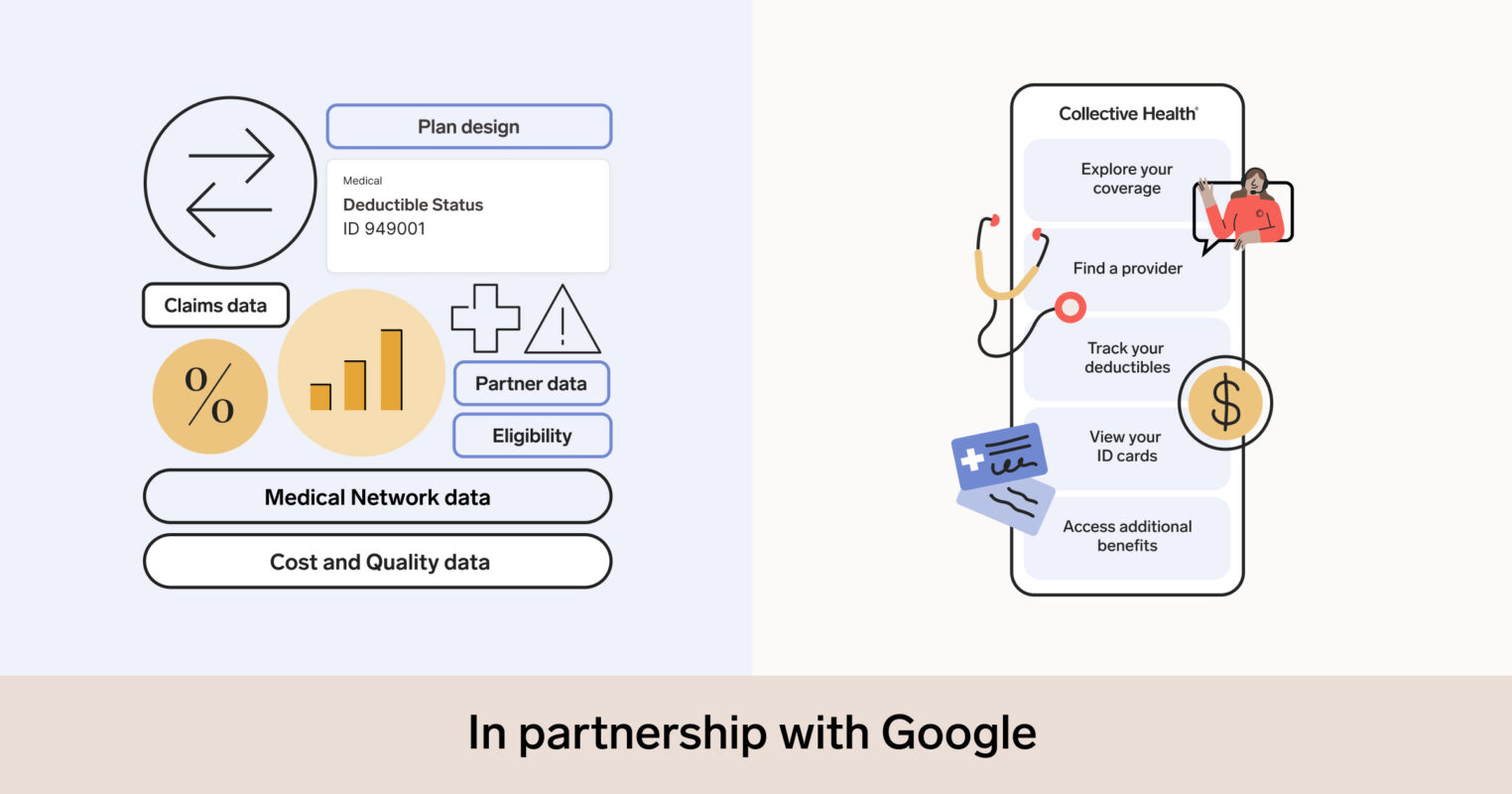
Identifying members in need and understanding their unique issues, including their socioeconomic circumstances, requires a delicate combination of technology and human interaction. To do this, Care Navigation brings together patent pending technology like CH Cortex™, Collective Health’s proprietary machine learning engine that analyzes different data sources including medical claims, with our in-house team of pharmacists, social workers, nurses, and dietitians to provide real-time, human support.