By Mara Kailin, Psy.D.
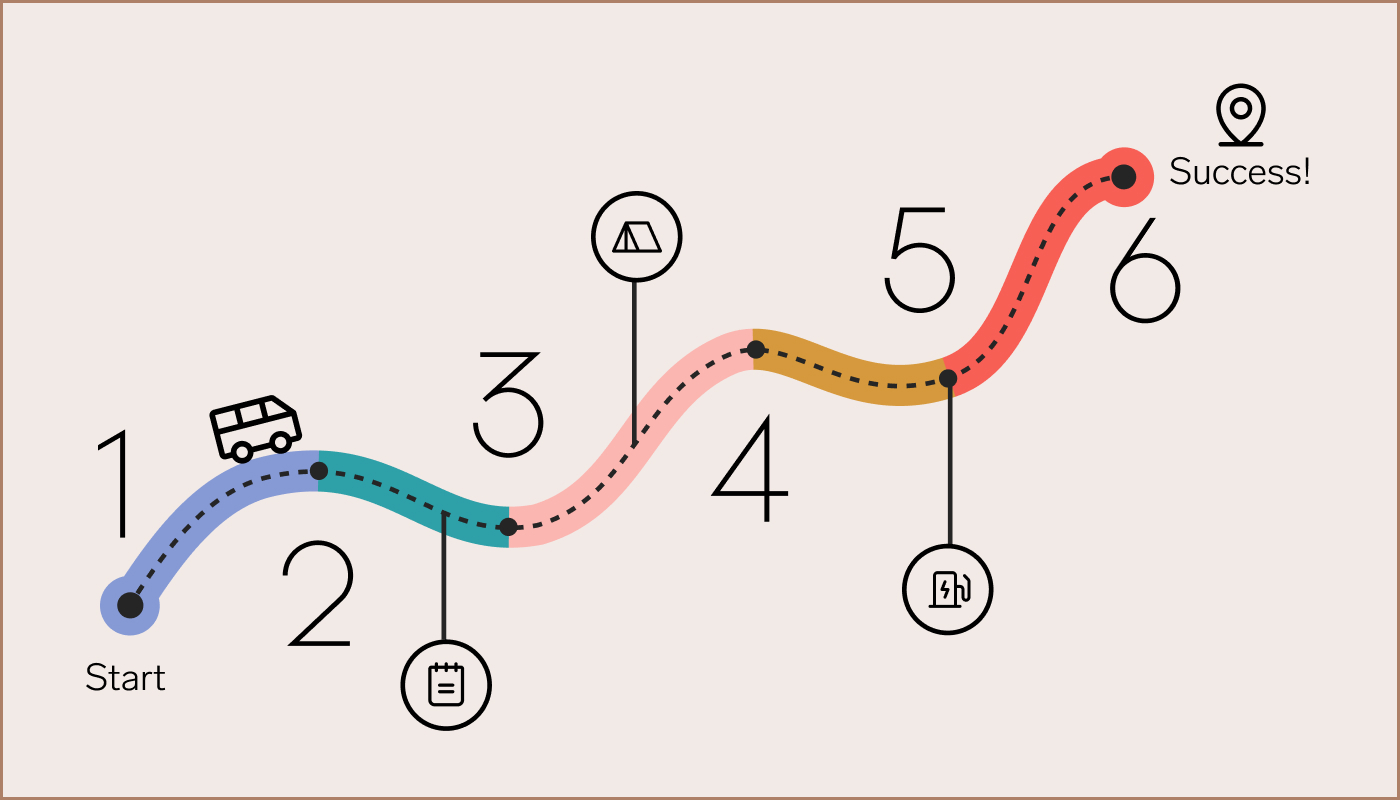
A person’s mental health journey rarely starts with a behavioral health expert. Often, it starts within the primary care setting, and many patients rarely follow up on a referral to a specialist.
If you have ever felt extremely anxious, you may have experienced nausea, light-headedness, or maybe even tightness in your chest. This is the physical connection between our brains and the rest of our bodies.
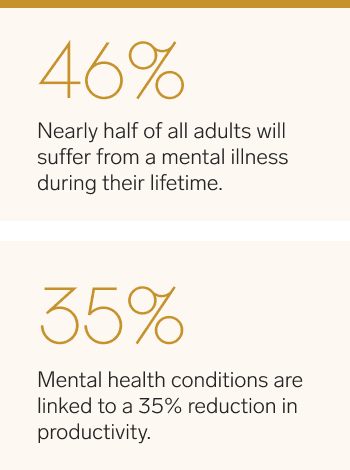
Mental health concerns can cause and contribute to physical conditions and physical ailments can cause and exacerbate psychological distress or disease. With almost half of adults (46.4%) experiencing a mental illness during their lifetime, this relationship between mind and body is becoming even more essential. However, much of the healthcare system is behind the times and treats the mind and body separately.
Primary care providers are often the first to identify mental health issues, and thus, are critical in facilitating access to behavioral healthcare for their patients. However, in most settings, patients are referred to an outside mental health specialist.
Research has also shown that when patients are provided an outside referral to access care at a later date, especially for something as sensitive as their mental health, many of them never end up following through. This is why treating mental illnesses within the primary care setting can vastly improve access to mental health care, reduce stigma and improve outcomes.
Find out more
Integrated approaches improve outcomes
Integrating mental health and primary care allows for a more holistic approach to treating mental health than the traditional consultative and referral models. Instead of making time to go to the doctor only to be referred to a specialist somewhere else, primary care physicians and mental health professionals can address behavioral and physical health needs collectively, building upon each team member’s skills and expertise.
A collaborative care approach is team-driven and evidence-based, and research has demonstrated time and time again that this integrated approach leads to more consistent and sustained patient outcomes and higher rates of patient satisfaction. This care model is patient-focused and holistic, resulting in better treatment adherence, as everyone works as a team to address both physical and mental healthcare needs.
With mental illness being one of the leading causes of disability in the U.S.—accounting for almost 19% of years of life lost due to disability and premature mortality—comprehensive, integrated care can detect a problem sooner before it heavily impacts a patient’s functioning and quality of life.
A holistic approach integrates brain and body health
When a person is diagnosed with heart disease, cancer or some other life-threatening physical illness, the patient may also develop symptoms of anxiety or depression. If left untreated, co-occurring mental health problems can severely impact a person’s ability to care for themselves and adhere to treatment requirements.
Primary care providers are often the first to identify mental health issues.
A study conducted on depression in cancer patients revealed that depression increases mortality rates by up to 39%. Even patients displaying only a few depressive symptoms can be at a 25% increased risk of mortality, and over 70% of oncologists believe that mood affects the progression of cancer.
Mental health conditions can also significantly impact workforce productivity; mental health conditions are linked to a 35% reduction in productivity, costing the US economy more than $210 billion in absenteeism, reduced productivity, and medical claims. This data is just a snapshot of the overwhelming research on the profundity of the mind-body connection.
Virtual care reaches more patients
The behavioral healthcare system has long been plagued by wide disparities in resources and access, with rural communities having the most significant provider shortages along with high rates of chronic illness. High quality telehealth options have opened up opportunities to address health inequities and some of the social determinants that contribute to them, such as stigma, transportation and lack of local providers.
At 98point6, patients are diagnosed and treated by a primary care physician and a mental health professional within the same care team. Together, the team determines the course of care and utilizes evidence-based treatments for body and mind.
Our model allows for more frequent upstream prevention and early intervention, saving patients from exacerbation of conditions and leading to more profound and sustained condition management and recovery.
By empowering patients to actively engage in their healthcare from a holistic standpoint, we can reduce the impact of absenteeism in the workplace, help people live healthier lives and see tangible improvements in their overall health and productivity levels.
Disclaimer: The views expressed in the article are those of third parties. They do not purport to reflect the opinions or views of Collective Health or its members.