At Collective Health, we’re on a mission to make healthcare easier to navigate and understand for everyone. We also realize that when we say everyone, we must also acknowledge that our current healthcare system isn’t designed to equally or fairly serve the needs of “everyone.” Which is why our Product and Customer Experience teams are working to find ways we can deliver more culturally competent services-services that more readily meet the evolving social and cultural needs of our members. Along with working toward our mission, creating a more culturally competent organization has proven benefits, including improved health outcomes, potentially lower costs and fewer care disparities.1 The first step to delivering more culturally competent benefits is making sure our members feel included and supported.
Here’s a preview of some of the ways we’re doing just that:
Problem: A recent survey found that over 35% of employed individuals reported not fully understanding the benefits they enrolled in during their most recent open enrollment period. That percentage went up even higher among millennials, with 54% saying they didn’t understand their benefit selections.
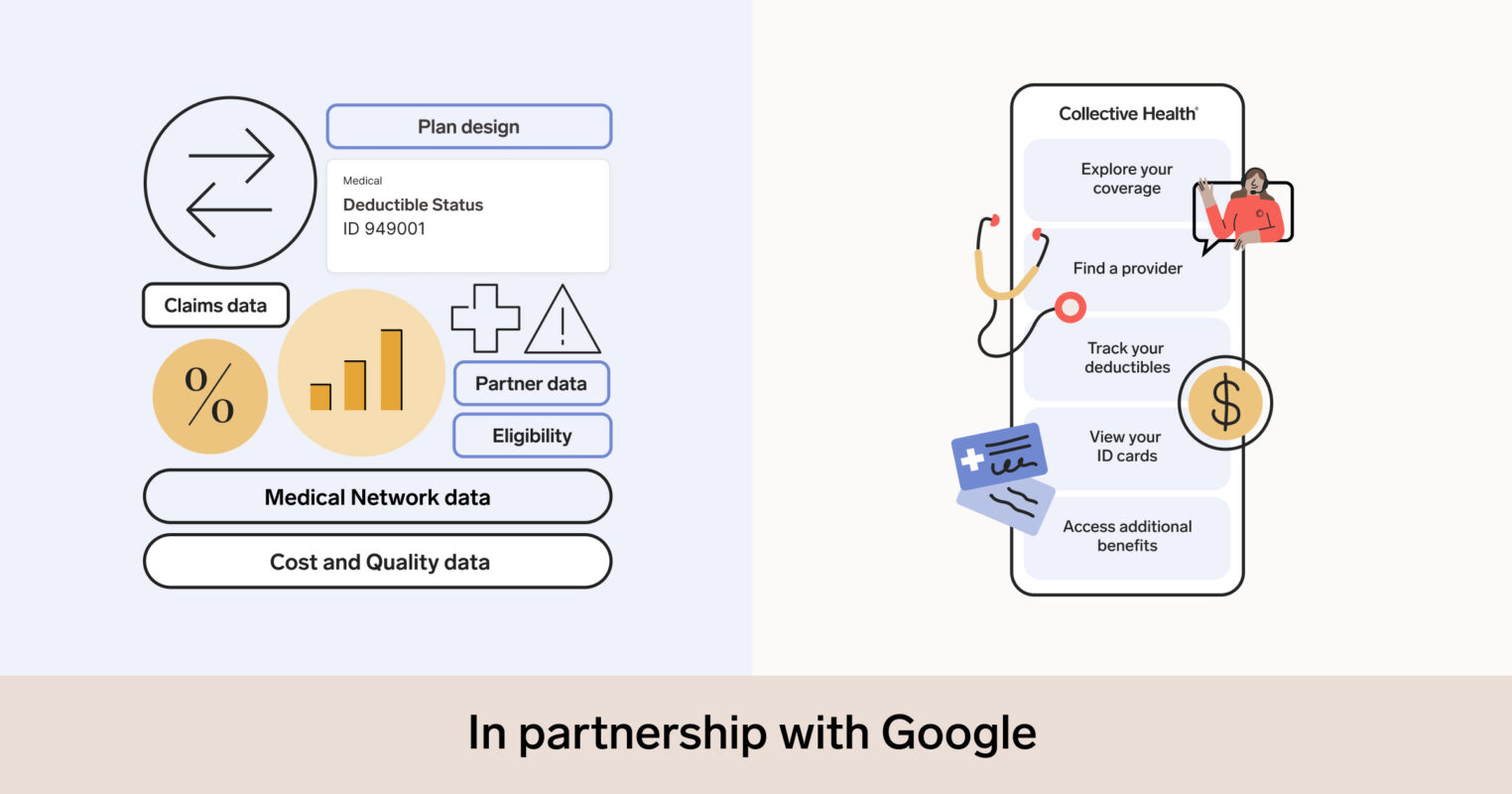
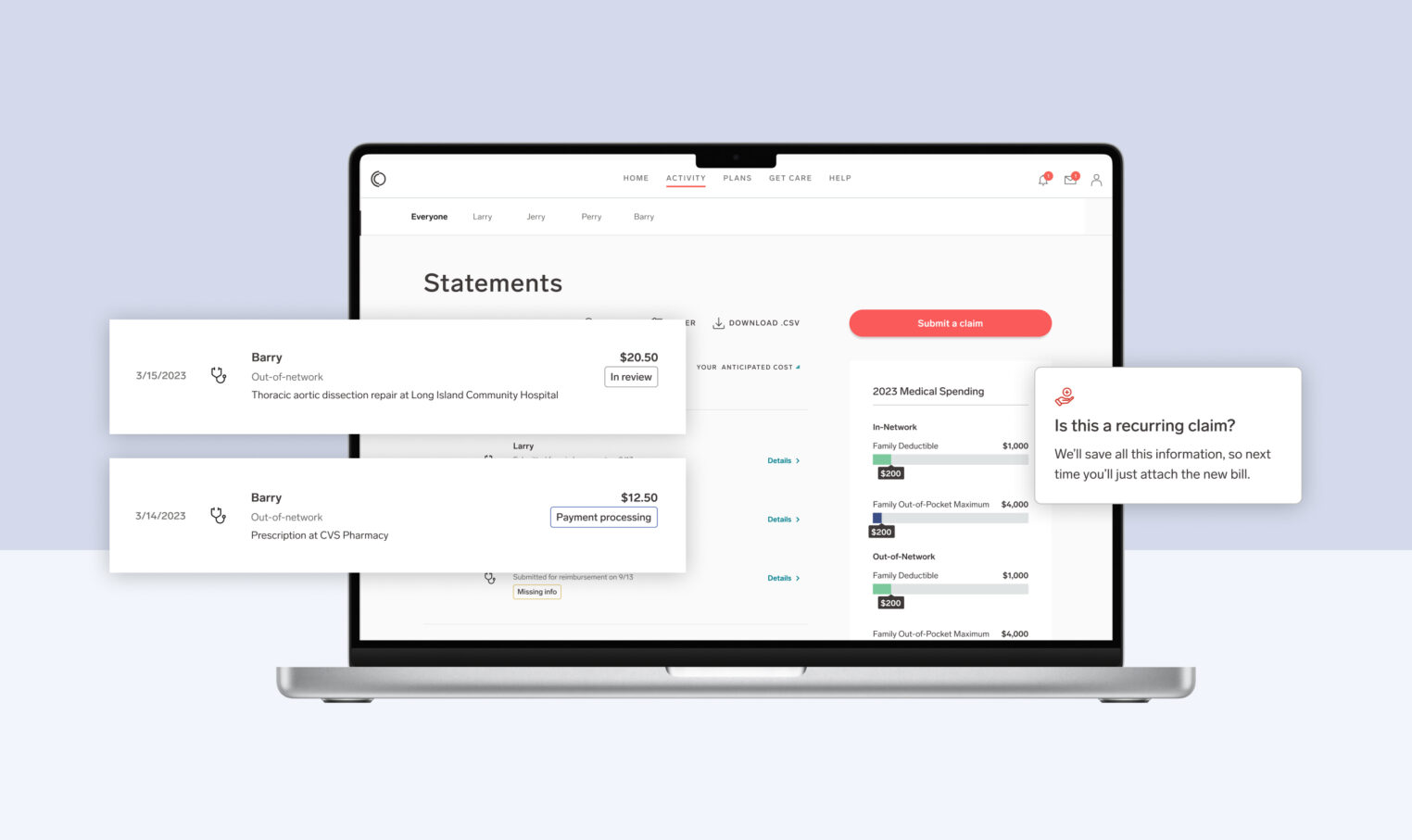
How we’re working to address it: At Collective Health, our mission is to make healthcare easier to understand and navigate—whether that means helping members discover specialized providers, using culturally competent language, or thoughtfully organizing health benefits so members can find what they need. We offer our customers a high-touch, human-centered experience called Collective Care™, which includes our personal member advocacy and navigation services, such as:
- Member Advocates: true experts in health benefits who provide members with thoughtful solutions to issues and help members navigate today’s confusing and cumbersome healthcare system with empathetic, respectful support that takes into account gender identity, sexual orientation, family, and ability.
- Care Navigation: our team of nurses, pharmacists, social workers, and dietitians, providing guidance and support for complex care needs. For customers that adopt this service, our Care Navigation team plays a crucial role in helping members receive the right support, at the right time, across a wide range of complex health needs. Care Navigation combines the use of data on social determinants of health in conjunction with our team of health professionals, who are well-versed in the dynamic psychosocial, pharmaceutical, and medical issues of at-risk communities, to reach members in need of comprehensive care coordination.
Problem: In a national survey2 conducted by the National Center for Transgender Equality, 23% of the individuals surveyed reported that they didn’t go to the doctor when they needed to out of fear of being mistreated as a transgender person. And nearly 33% of the respondents reported negative experiences when seeking care, like being refused treatment because they were transgender.
How we’re working to address it: At Collective Health, we have a number of ways our team is working to ensure our transgender member population is included and supported through their benefits experience:
- My Collective™, our personalized app and interface that makes it easy for members to manage their health benefits, from wherever they are, includes a dedicated page for information about any gender affirming and transgender services offered by their plan. Members can see all their plan benefits including applicable counseling, prescription hormone therapy, and gender reassignment surgery.
- Our Member Advocates receive training on Transgender Health, including common terms, best practices, resources and what transgender care means to our members.
- We offer the option to support gender-neutral benefits in claims adjudication, so that members can receive the screenings and other services they need.
- We can work with your plan’s medical network to help adjust prior authorization criteria for cosmetic services to reduce friction.
Problem: Research shows Black, Indigenous, and people of color (BIPOC) have greater barriers when it comes to accessing mental health care — for a variety of reasons, including racism, discrimination and lack of provider concordance (with the majority of mental health providers being White). Recent research3 also shows that people have better experiences with their providers when they share the same race or ethnicity.
How we’re working to address it:
Our Member Advocates have access to our Get Care tool and several publicly-available resources to help members search by specialty, location, name, and language, to connect with a provider of their needs. Searches are performed at a member’s request, in a non-discriminatory manner and in protection of our member’s care. As part of this, we also reference many unaffiliated associations such as: the Association of Black Psychologists, as well as other resources like the National Queer and Trans Therapists of Color Network. In addition, Member Advocates can help to confirm whether those providers are in-network to help members potentially avoid unnecessary out-of-network costs.
There’s still a lot of work to do within the industry to more effectively address inequities in healthcare. Here at Collective Health, our teams are dedicated to helping our members understand and navigate today’s confusing and fragmented healthcare system, and, as part of this, we continue to evaluate and expand our services to meet the evolving social and cultural needs of our members.
Want to learn more? Download our Inclusive Member Support Guide to see how we deliver care that aims to meet the needs of your entire member population.
2: James, S. E., Herman, J. L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality.
3: Takeshita J, Wang S, Loren AW, et al. Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings. JAMA Network Open. 2020;3(11):e2024583. doi:10.1001/jamanetworkopen.2020.24583