Today on the blog, Dr. Louis Dickey, Medical Director at our Premier Partner Hinge Health, discusses 4 ways musculoskeletal health programs can help employers to reduce care gaps and improve health equity.
The COVID-19 pandemic has brought many healthcare issues to the forefront, including health inequities. Across the board, researchers have found that individuals with lower incomes, rural residents and people of color experience worse health outcomes. This dynamic is true for numerous chronic health conditions, including back, neck, knee and other joint pain conditions.
Many employee benefits leaders and health plans are turning their attention to musculoskeletal (MSK) conditions, with the goal of reducing care gaps for every segment of their workforces. As a first step, they are evaluating social determinants of health and then designing MSK programs that take these factors into account.
Hinge Health, a digital MSK clinic that combines advanced sensor technology, computer vision, and a full clinical care team has released a free eBook to help benefits leaders understand and address MSK conditions affecting employee populations: Addressing Disparities in Musculoskeletal Care: How Employers Can Narrow The Health Equity Gap. Here are the highlights from our findings.
Find out more
How Social Determinants of Health Affect MSK Care
Social determinants of health can have a negative impact on MSK care. It’s widely recognized that race and ethnicity lead to poorer health outcomes. The National Academy of Medicine found that ethnic minorities consistently receive lower-quality healthcare than whites, even after taking insurance status, age, income and severity of disease into account.
Travel and transport barriers
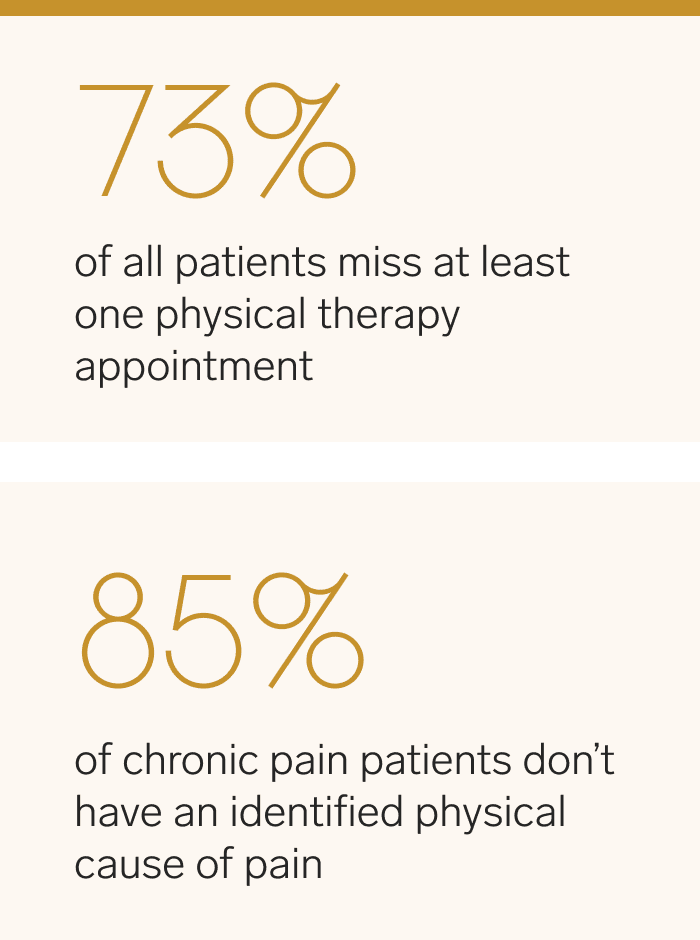
In addition to race, other factors also contribute to poor outcomes for MSK conditions. For example, access to care is a persistent problem for individuals with MSK conditions. Studies show that 73% of all patients, rural and urban, miss at least one physical therapy appointment. For individuals living in rural areas, the distance to clinicians often hinders access to care. It’s common for rural patients to drive as long as forty-five minutes each way to a PT appointment and some drive as much as four hours in a day to reach a physical therapist’s office.
On top of the distance to clinicians’ offices, access to transportation can also make it difficult for people to get to medical appointments for their MSK issues. The American Hospital Association reports that transportation challenges prevent 3.6 million Americans from receiving medical care each year. Access to reliable transportation is problematic for one in five patients residing in rural areas. When lack of transportation results in missed, canceled or delayed appointments, continuity of care is interrupted and successful management of medical conditions is compromised.
Income disparities
Income is another social determinant of health that has a profound impact on the treatment of MSK conditions. In-person PT can be particularly challenging for hourly shift workers who must take unpaid time off from their jobs to drive to PT appointments several times a week for many months. In addition, many lower-income workers are unable to afford high deductibles for numerous in-person PT appointments. Once people drop out of PT, their MSK condition can worsen and they might turn to opioids and surgery as their last resort.
Education and health literacy
Health literacy and education play a critical role in MSK care, but nearly one in three American adults have low levels of health literacy, with disproportionately low rates among lower-income individuals who are eligible for Medicaid. People with MSK conditions and low levels of health literacy may be unaware of their treatment options.
Education can help patients better understand the neuroscience of pain and demonstrate that surgery isn’t always the best course of action for MSK issues. This is especially true for people with chronic pain since we know that 85% of them do not have an identified physical cause of their pain, so interventions that focus on a physical cause of the pain are frequently ineffective and unnecessary.
Read now
Four Ways Employers Can Improve Health Equity in MSK Care
Once employers understand the social determinants of health that affect MSK care, they can adopt new approaches to MSK care that close health equity gaps for their workers. Here are four examples of programs that leading organizations are deploying:
1. Improve access to care with comprehensive digital technology
Digital MSK solutions take care directly to employees’ homes. This enables individuals to access care via a digital platform in a place that is most convenient for them. Hinge Health’s Digital Musculoskeletal Clinical, for instance, pairs a complete clinical care team with a comprehensive suite of digital technologies.
2. Offer zero out-of-pocket costs with a Digital MSK Clinic
For members living in underserved communities, employers must focus on increasing awareness about MSK care and increasing access to low-cost options. Digital MSK care with zero out-of-pocket costs removes financial barriers to conservative care, particularly for populations that need it most.
3. Personalize care with a complete clinical care team
To create a more equitable healthcare system, it’s important to understand a patient’s logistical barriers to care, as well as their social and familial beliefs about what optimal care looks like. Treating the whole person means understanding each person’s unique situation, barriers and beliefs. Hinge Health’s complete clinical care team includes doctors of physical therapy, health coaches, physicians and orthopedists. Health coaches help participants recover based on their unique obstacles, environment, and goals.
4. Enhance health literacy through education, real-time data, and expert medical opinion
When members are unaware of their MSK treatment options, they may assume that surgery is the only course of action. Hinge Health’s in-house orthopedic surgeons offer free expert medical opinion. Of Hinge Health participants who get an expert medical opinion, seven in 10 chose lower-cost, less-invasive care. Education about the linkage between MSK pain and other aspects of health like depression, stress, anxiety and diet can also help individuals take a more holistic approach to improving their lives and getting back to the activities that they love.
As benefits leaders and health plans design more equitable and inclusive healthcare benefits, many are turning to Hinge Health to address employees’ MSK conditions. To learn more about how Hinge Health can support your organization and do the same, download our white paper.
Disclaimer: The views expressed in the article are those of third parties. They do not purport to reflect the opinions or views of Collective Health or its members.