78% of employees said they are more likely to stay with their employer because of their benefit program. With a well-managed benefits program, companies can help attract new talent, improve retention, and foster a long-term team environment. A smooth-running benefits program can also help employees stay healthier and even be more productive.
There’s just one issue: on a whole, modern healthcare benefits systems are broken. Not broken like a car with a snapped axle. Most healthcare plans will — eventually — let your members reach their destination.
But broken like a car that runs on five cylinders instead of eight, nearly stalling and then backfiring when you try to accelerate. Broken like a car whose radio only plays jazz show tunes as you wait in endless traffic.
The structure of modern benefits plans can lead to confusion and frustration. The result may be that your employees don’t understand their healthcare benefits well. Some may even be avoiding important healthcare needs because the whole system feels like the car nobody wants to drive.
But it doesn’t have to be this way. Collective Health is transforming the benefits experience from outdated and disjointed to frictionless and easy to understand with a centralized digital ecosystem where your employees can get information and support in one click.
Download this report now
The root of the problem: disjointed, fragmented services
If you stub your toe on the coffee table, you call one number. If a tooth hurts, you call a different number or log into a different website or app. And if you lose your glasses, you call a third number, assuming you can find the number without your glasses. If you lose your glasses and stub your toe, your plans for the entire afternoon just changed.
The benefits structure feels disjointed, and that’s because it often is. But why? Parts of the current state of healthcare plans are simply borne of a prior era. Other parts were decided by committees — and we all know how that goes.
In many cases, things are the way they are because nobody tried to make the experience better and because that’s the way it’s always been. Yes, often it really is that simple. The benefits industry is still very traditional, in the sense that many providers have yet to effectively leverage the power of technology to create streamlined member experiences.
It doesn’t have to be this way.
Imagine support wait times measured in seconds rather than the 40-minute average for the industry. Imagine one number to call, whether your toe hurts, your tooth hurts, or your glasses have gone missing (again). Collective Health can help. We know just how challenging this industry is to navigate, which is why we’ve made member experience core to our offering.
“Healthcare and insurance concepts are hard to grasp, even with so many resources out there. Whether it’s with open enrollment materials, tooltips in our products, or member outreach, we constantly think about how our content can be both immediately useful, helpful, but also inspire people to learn more and feel empowered,” explains Brian Bagel, Senior Manager, Content Design at Collective Health.
How to create a personalized healthcare member experience
Although we all have a member number within our healthcare plans, nobody wants to feel like a number. There’s a unique opportunity to make the experience better through technology and a cohesive support system that works efficiently and builds loyalty. Here are the three key areas to focus on if you want to improve member experiences:
1. Health benefits information should be easy and accessible
Healthcare plan documents often rival 1040 tax instructions for dry reading guaranteed to confuse everyone. Jargon-heavy plan literature creates a barrier to entry, making it difficult for members to choose the right coverage or understand what’s covered.
Too many options without a clear definition of what each choice means and how it might affect real-world healthcare needs can leave employees confused about their options — even when the coverage meets their needs.
Plan choices like deductibles, copayments, and maximum out-of-pocket costs all play a crucial role in choosing the right plan, but may not be explained in a way that people outside the benefits industry understand easily.
The result is described as choice paralysis in which employees can’t choose a plan that works well for their unique needs. Instead, they might just pick a plan at random rather than choosing options well matched to their situation.
Fortunately, there’s a solution. Collective Health helps members easily navigate plan choices, with tips on how to choose what’s right for you. We write plan details in plain English.
At the heart of it all, the Member Benefits Statement (MBS), also known as an Explanation of Benefits (EOB), shows what the plan covers as well as which costs the member pays. For a truly personalized member experience, the MBS must be easy to understand.
At Collective Health, our Member Benefits Statement is designed to be straightforward and accessible, modeled after a credit card statement. It was developed using extensive customer research to cut through the jargon.
2. Getting help should be simple and fast
Operator, please. Can I speak to a real human? Call waiting is a common problem and even without jazz music on hold, and there’s nothing personalized about the experience at all.
How many members avoid using benefits for situations that affect their health because it’s nearly impossible to get a real person on the line. How many start to feel that maybe their benefits plan isn’t as good as it could be or just isn’t a good fit for them?
Remember, 78% of employees said they are more likely to stay with their employer because of their benefit program.
At Collective Health, members get connected to a helpful human in just under 30 seconds. Our Member Advocates are the only point of contact for members, so they can spend their time actually resolving issues, not transferring you to another number.
Healthcare is personal and convenience is essential. Collective Health Member Advocates are available via phone, email, and online chat. Members also have 24/7 access to the Help Center, a database of relevant information, frequently asked questions, and educational resources.
3. One hub for your health benefits
With connected print, digital, and human support, members have one place to go for their health benefits.
In many cases with traditional benefits programs, members have to use one app or website for medical needs, another for dental, a third for eye care, and possibly a fourth for prescription needs. That alone sounds like a recipe for frustration and the exact opposite of a personalized healthcare member experience.
The member experience can seem disjointed — because it is — if each of these resources is an island unto its own. Often, health insurance apps are also difficult to navigate. And there may even be several websites or apps to use for a single healthcare need, with none of them working the same way.
Collective Health has integrated healthcare services for your plan into one platform, convenient to access at home or on the go using our website or mobile phone app. Looking for an in-network dentist, primary care physician, or optometrist? Then, as a member, you have just one place to search for the care you need.
Benefits of a personalized healthcare member experience
Imagine a world in which healthcare choices are simpler to understand and adapted to individual needs, empowering members to make well-informed decisions.
Imagine a healthcare plan that resolves issues efficiently and puts members first with lightning-fast support by phone, chat, or email.
Would your employees be more likely to access their benefits? Would your workforce become healthier overall, and feel their benefits program offers real value? Would your members be more likely to stay as a productive part of your team, helping reach new goals for your company and for themselves?
A benefits system that puts members first offers a personalized healthcare experience that can ultimately support productivity, employee satisfaction, recruitment, and retention.
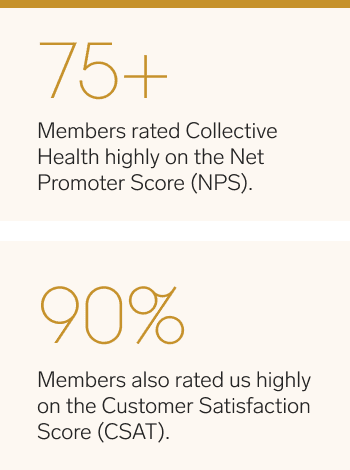
At Collective Health, our goal isn’t to get members off the phone as quickly as possible; instead, we work on understanding and resolving the root of their inquiry. That’s why we focus on Net Promoter Score (NPS). NPS is a really powerful (and unforgiving) metric.
It’s scored on a -100 to +100 scale, with the average for the health insurance industry scoring only 8. Collective Health scores 75+ as a Net Promoter Score, rivaling customer-focused companies like Apple, USAA, and Amazon.
Is it time to transform your member experience?
Traditional healthcare benefits systems are built on decades-old practices that can create a barrier between members and the best healthcare options. By extension, this experience can create barriers between a company and its employees.
A personalized healthcare member experience can help foster a spirit of teamwork, with members feeling well-supported by healthcare benefits that are easy to access and easy to understand.
Learn more about Collective Health and how we can help you deliver seamless benefits that power your business and empower your people with one of our webinars.