A perspective by Jen Nishio, Head of Strategic Accounts & Alliances
Most benefits leaders agree that the member experience is key to the success of benefits programs—when our people are happy, our jobs are both much easier and infinitely more satisfying. But often we feel powerless to create the member experience our people deserve in the face of systemic problems beyond our control. I joined Collective Health after working as a benefits manager (and, prior to that, a consultant) for nearly a decade with the goal of being a catalyst for helping people have better healthcare experiences, both as a member and as a benefits leader. I had seen firsthand that people struggled with their benefits and I wanted to fix the problems they encountered. Problems such as:
- Frustrating member experiences: It was disheartening seeing people try to solve problems with limited tools, resources, and customer support—eventually giving up in frustration and turning to me to resolve their challenges.
- The litany of “no”: No matter how confusing it was for members, it seemed impossible for the “system” to improve things. As a benefits leader, I was constantly being told things were impossible. “The system can’t handle that” or “We can’t process it this way” was the response.
- Lack of empathy: My biggest challenge was seeing how dismayed my people were with the lack of empathy in the system. Too many members of my population felt lost and left out in the cold—whether they were trying to find an in-network doctor or just understand a bill.
As a benefits leader, I was constantly being told things were impossible.
The Collective Health member experience is designed to help members have a direct and trusted relationship with their health plan, so they can find exactly what they need without creating additional work for themselves or benefits professionals. To do that, we’ve prioritized four key areas:
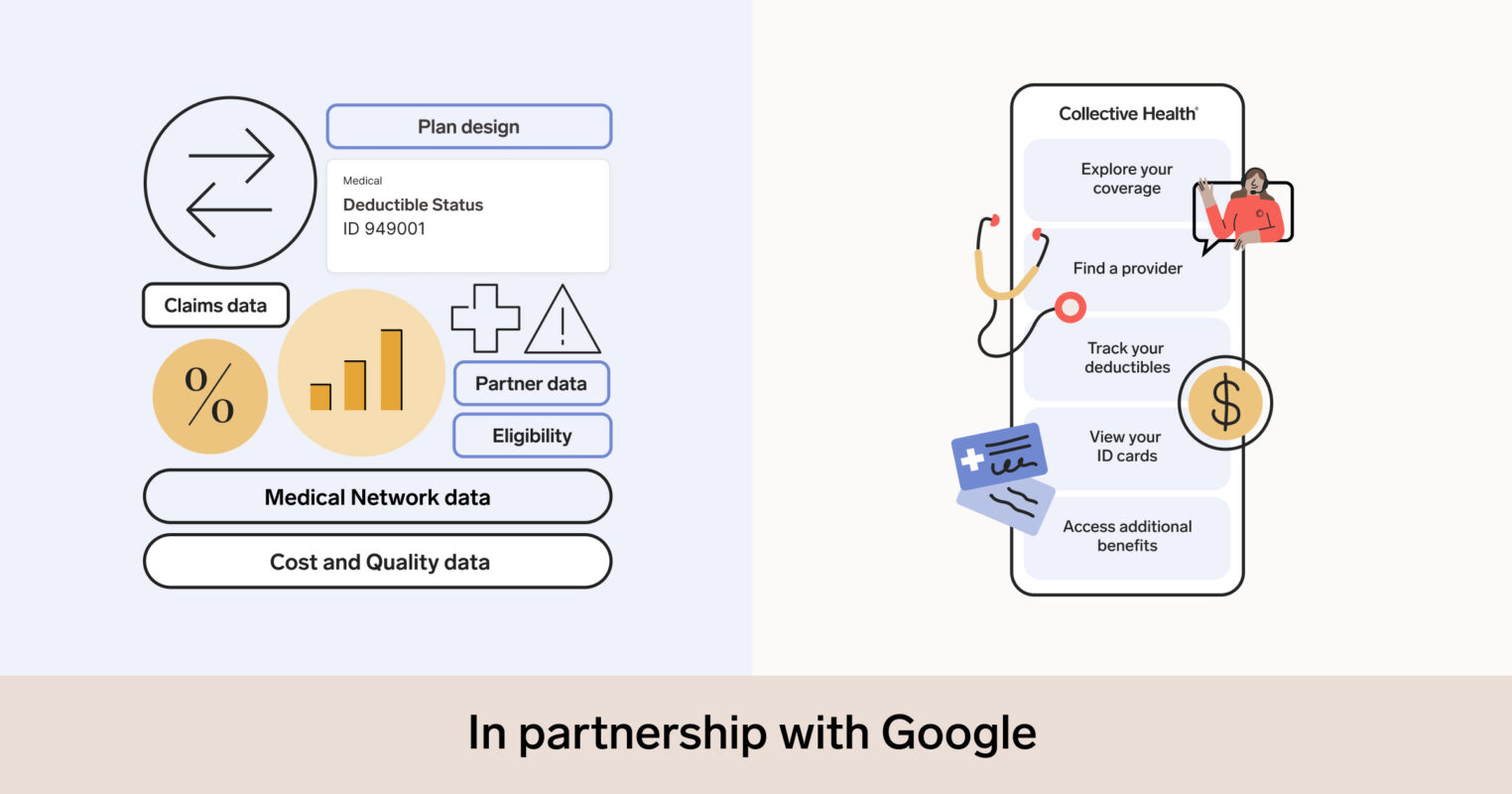
- Choosing the right plan: One of the areas members find most challenging is navigating their plan selection. Typically, benefits teams spend hundreds of hours creating Open Enrollment communications, presentations, summaries of what is changing and staying the same, and more. With Collective Health, plan details are presented in clear and meaningful language on both our website and mobile app—nothing gets lost in translation.
- Finding the right care: For many members, finding medical, dental, and vision providers can be very confusing. On the Collective Health platform, we have just one search bar that only shows in-network providers for the specific networks and plans your employer has chosen. You no longer have to hunt through multiple websites. We take the guesswork out of remembering what plan or network you’re on, making both Open Enrollment and finding a doctor much less painful.
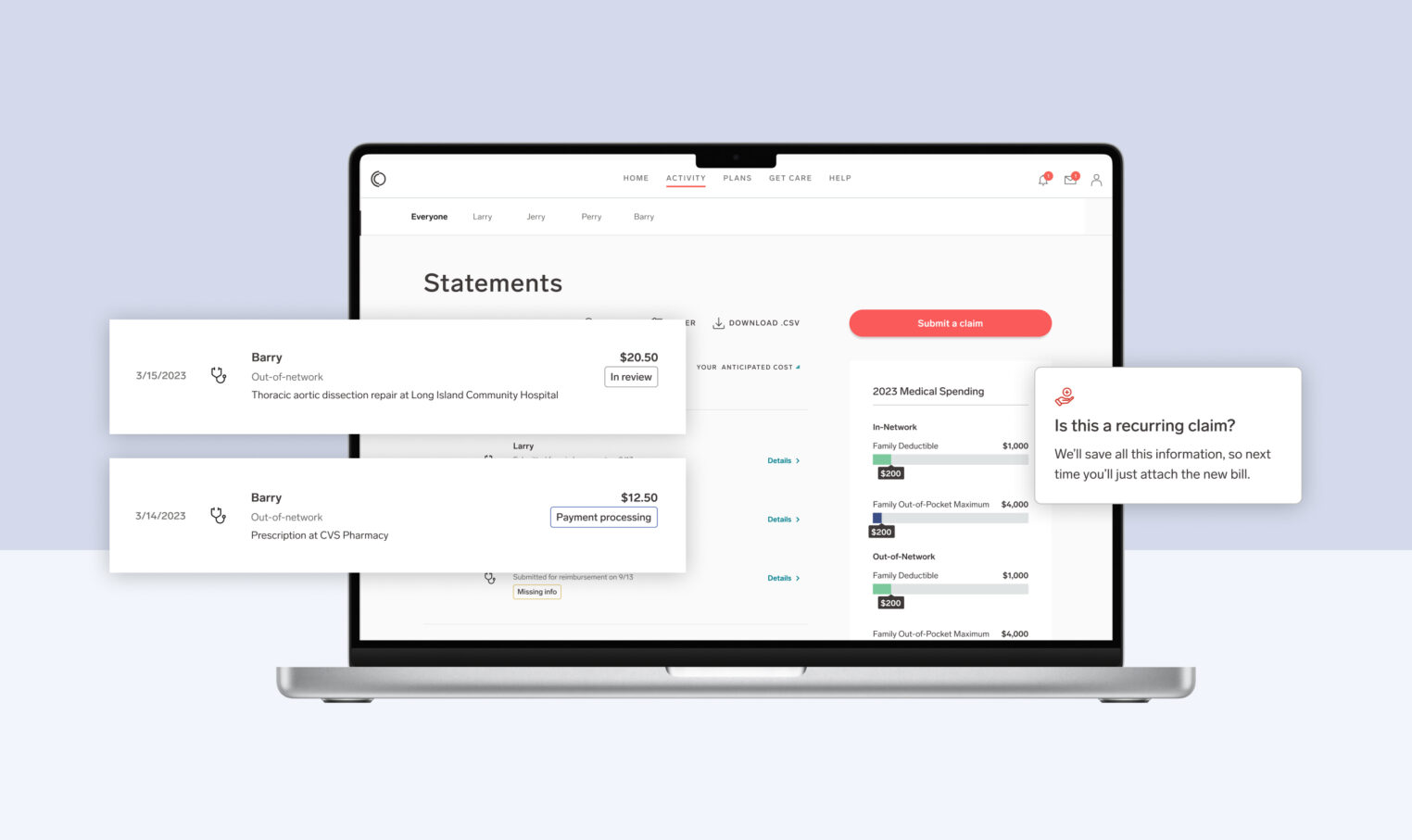
- Understanding your coverage: Our Explanation of Benefits (EOB) are designed to be straightforward and accessible. When you compare your EOB to the bill you get from your doctor, it should be pretty easy to figure out how they line up. If it isn’t, it’s not a problem—you can always call, live chat, or email a Member Advocate to get your questions figured out quickly.
- Providing a human touch: People need care at important times in their lives: they have a scary diagnosis, a fresh injury, or they’re having a baby. Health benefits should work for everyone—from those who have minimal interaction with providers to those who have serious health issues and are navigating complex situations. Our Member Advocates know that it’s their most important job to help relieve additional stress for our members at what can be a very confusing time. When you work with Collective Health, you partner with real people who are knowledgeable and empathetic, backed by a system infrastructure that empowers them to help people when they need it.
My favorite thing about the Collective Health member experience is that we meet people where they are. We do this by communicating with people in whichever format they prefer—email, chat, or by phone—and we use simple and direct language, just like a benefits leader would do if an employee stopped by her desk. As a member recently shared:
“I have never had such a simple, straightforward, and productive experience with an insurance company’s customer service. I feel that this is a great example of Collective Health following through on what it claims to be (a new standard for the member experience). Thank you!!”
-Collective Health Member
For more on the design of the Collective Health experience, check out our new Member Experience video.