For most companies, a small number of employees account for a disproportionate amount of healthcare costs, typically driven by those dealing with chronic or serious illnesses. By Collective Health’s estimation, 10% of members account for 75% of spending. Without dedicated support, this cost imbalance can have an outsized impact on the companies providing health insurance as well as the individuals and families dealing with these health issues.
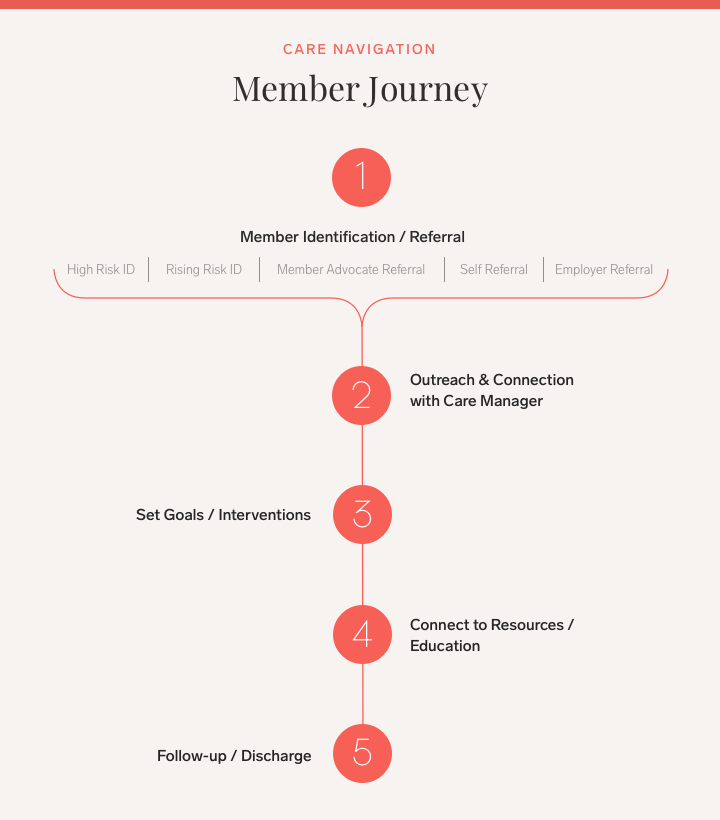
At Collective Health, Care Navigation plays a crucial role in helping people get the right support, at the right time, across a wide range of complex health needs. Care Navigation is a comprehensive care management program made up of our team of pharmacists, social workers, nurses, and dietitians that support people dealing with chronic or serious illnesses by guiding them on their journey to help them understand and navigate the disjointed U.S. healthcare system.
As Care Navigation has grown and evolved over the last few years, we’ve identified several areas where traditional care management programs often fall short, and which we aim to solve with Care Navigation. This includes:
- Outreach to people in need of high-touch care is delayed and often occurs after it would have been most impactful
- Trust issues persist between traditional health insurers and their members, which drags down member engagement in the programs
- Staffing issues and/or care management representatives are not always capable of addressing the dynamic psychosocial, pharmaceutical, and medical issues people are dealing with
Our Approach to Care Management
Complex health issues are often a result of socioeconomic factors, and it’s why we put an emphasis on social determinants of health—for example, how members’ geographic location impacts their access to food or transportation—as part of Care Navigation.
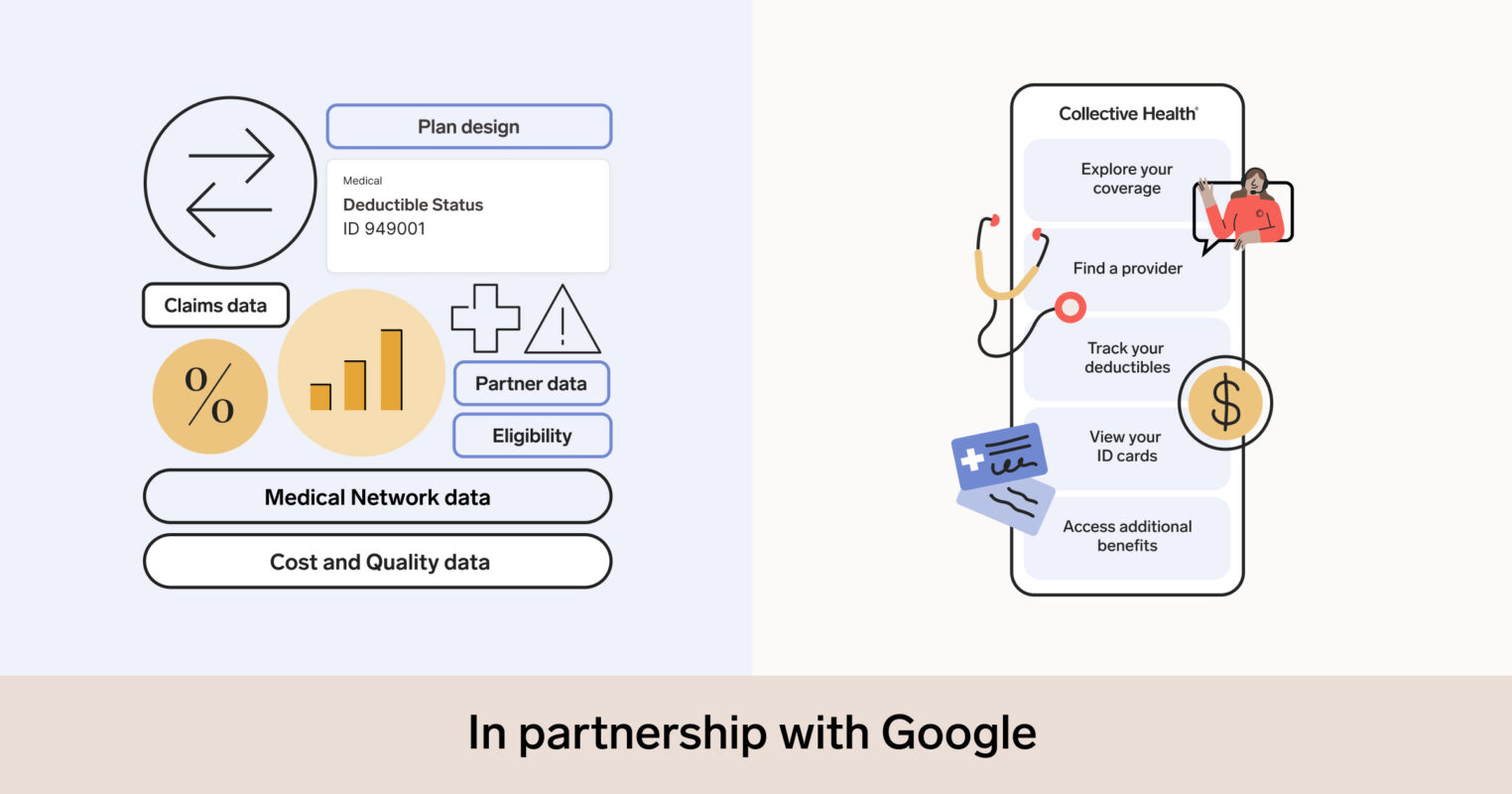
Identifying members in need and understanding their unique issues, including their socioeconomic circumstances, requires a delicate combination of technology and human interaction. To do this, Care Navigation brings together patent pending technology like CH Cortex™, Collective Health’s proprietary machine learning engine that analyzes different data sources including medical claims, with our in-house team of pharmacists, social workers, nurses, and dietitians to provide real-time, human support.
We continue to invest in both the technology and Care Navigation team in order to find the right balance for our care management solution, intentionally keeping our approach simple and rooted in three core principles:

This three pillar approach allows us to create a journey for our members that guides them in a way that best fits a particular individual’s needs. A closer look at each:
- Identify: Research shows that we need to identify members as soon as possible before they become at risk of incurring high healthcare costs. We use various data sources to do so, and this results in our ability to intervene early to maximize our impact.
- Build: Trust is critical, and without it, this program doesn’t work. Collective Health has spent the last seven years building trust with our members, reflected in an average NPS score of 70+ (vs the health industry average of 9).
- Intervene: We’re very deliberate about communications, and take into account member preferences while using a combination of digital and human outreach to ensure we’re able to engage with our members in a way that works for them.
Not Your Average Care Management Program
Here’s a snapshot of what this journey looks like for members, and the different steps we help define:
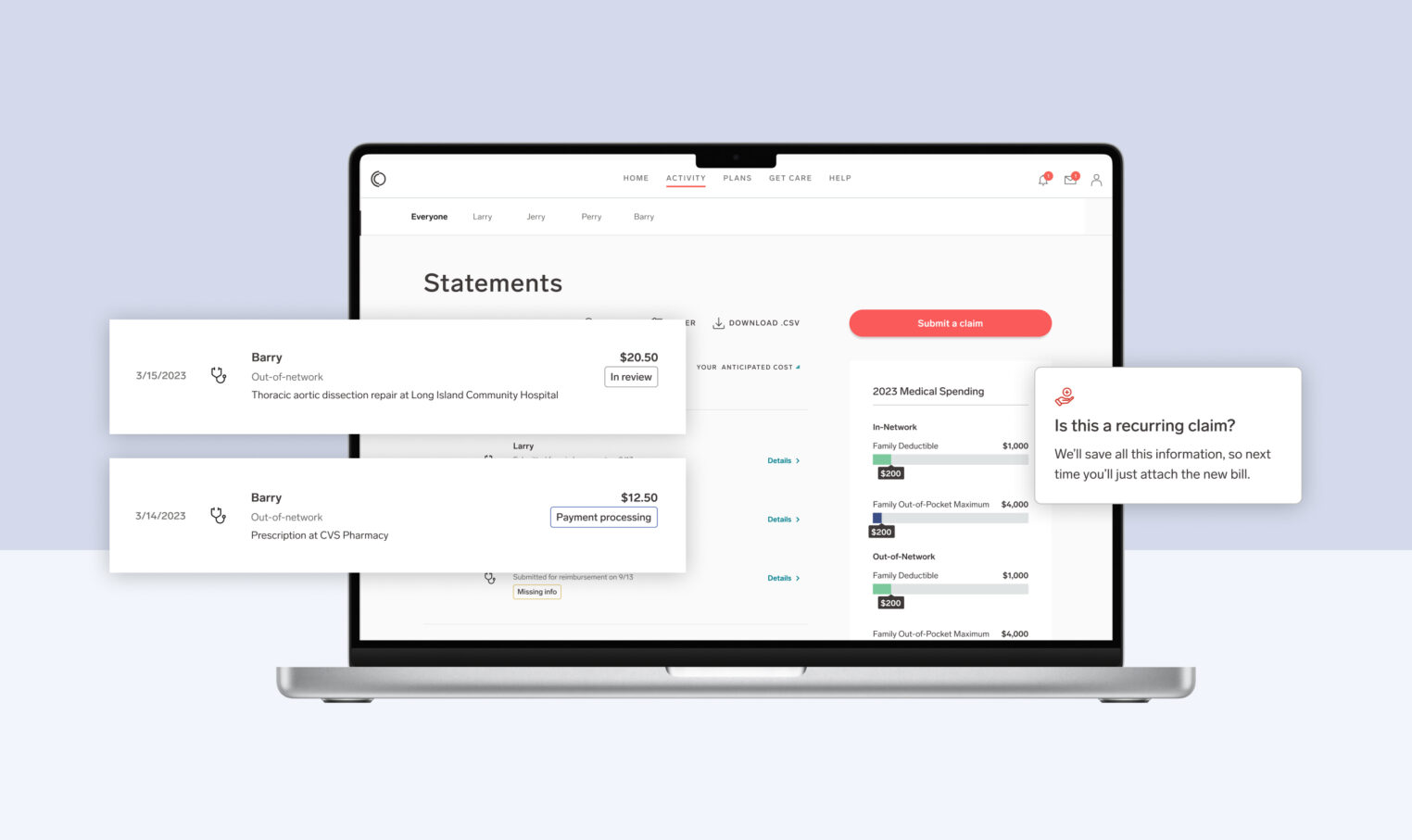
We value working closely with our members, customers, and consulting partners to understand their unique needs and provide them with a care management experience that truly makes a difference. That’s why it’s imperative we apply rigorous analysis around the effectiveness of our Care Navigation program, and the ways in which we’re supporting members with complex care needs, while also helping clients get more out of every dollar spent on care management.
Below is a view into the initial success of the program, examining some early analysis and the results of pharmacist interventions as part of Care Navigation.
Case Study: Pharmacist Intervention Through Care Navigation
Objective
Assess the return on investment of our pharmacist interventions conducted through the Care Navigation program, in monetary and clinical terms.
Process
Several hundred members participating in Care Navigation were analyzed during the quarter prior to and following contact with pharmacists. Members who received pharmacist interventions during 2019 and the first quarter of 2020 (15 total months) were then matched to control group participants in a commercial reference claims data repository.
Outreach by Care Navigation pharmacists—including by phone and digitally—was guided by a few factors including: high-cost claimant status, new high-risk diagnosis, pharmaceutical or procedure costs on claims, emergency room or hospital use, referral from a member advocate, or direct member request for assistance.
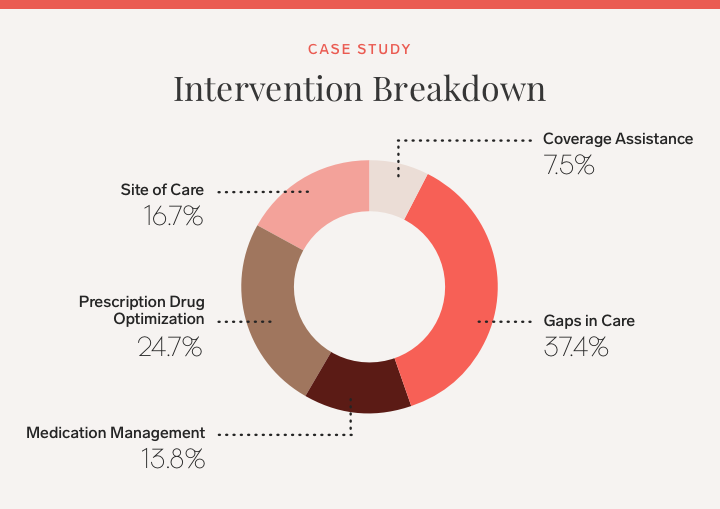
Interventions by pharmacists were classified into five categories.

Results
Over the course of 15 months, our Care Navigation program—specifically, pharmacist interventions as part of Care Navigation—drove health cost savings of $10.38 per employee per month (PEPM) across the entire program. This resulted in ~$5 in total PEPM savings against the Care Navigation program fee ($5.30 PEPM), providing roughly a 2:1 ROI for clients paying for Care Navigation.
For the population exposed to the pharmacist intervention, we saw $346 in net total savings on a PEPM basis.
Projection: For a client with 50 members engaged in Care Navigation pharmacist interventions, we estimate $207,600 in overall member population savings to the client on an annual basis.
Going a bit deeper: Of the hundreds of interventions by Care Navigation pharmacists, 29% had claims showing the intervention was successfully followed by participants. The majority of successful interventions were for Gaps in Care, which included a pharmacist reaching out to identify important health procedures or actions (for example, mammograms and colonoscopies) that people may be past due on receiving based on their health history. Full breakdown of the successful interventions:
If you’d like to learn more about Collective Health and our Care Navigation program, please reach out by filling out the below form.