These days, it feels like the soundbite, “our healthcare system is broken,” is playing on loop.
If you’re a benefits leader, you face it every day. Eligibility files break. EOBs don’t make sense. Members get lost in phone trees. You don’t get the data you need until six months after you need it. Not to mention the ~$305 billion the industry wastes every year on errors alone.
What’s the deal? Healthcare has a technology problem.
Health insurance is stuck in the 1980s. It runs on 40-year-old systems that weren’t designed to share data, work together, or learn from one another. As a result, we’re left with all of these disconnected pieces and incredibly frustrating experiences.
It’s about time we completely rethink and rebuild how health insurance works.
That’s what we’re doing at Collective Health. With a team of engineers, data scientists, and product designers, we built a modern health benefits infrastructure specifically for self-funded employers. Everything from eligibility management and claims processing to data analytics and information security—it’s big, and we’re all in.
Our approach comes down to four key themes:
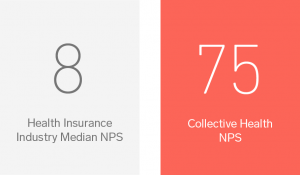
Collective Health has the most satisfied members in the industry, according to Net Promoter Score (NPS)
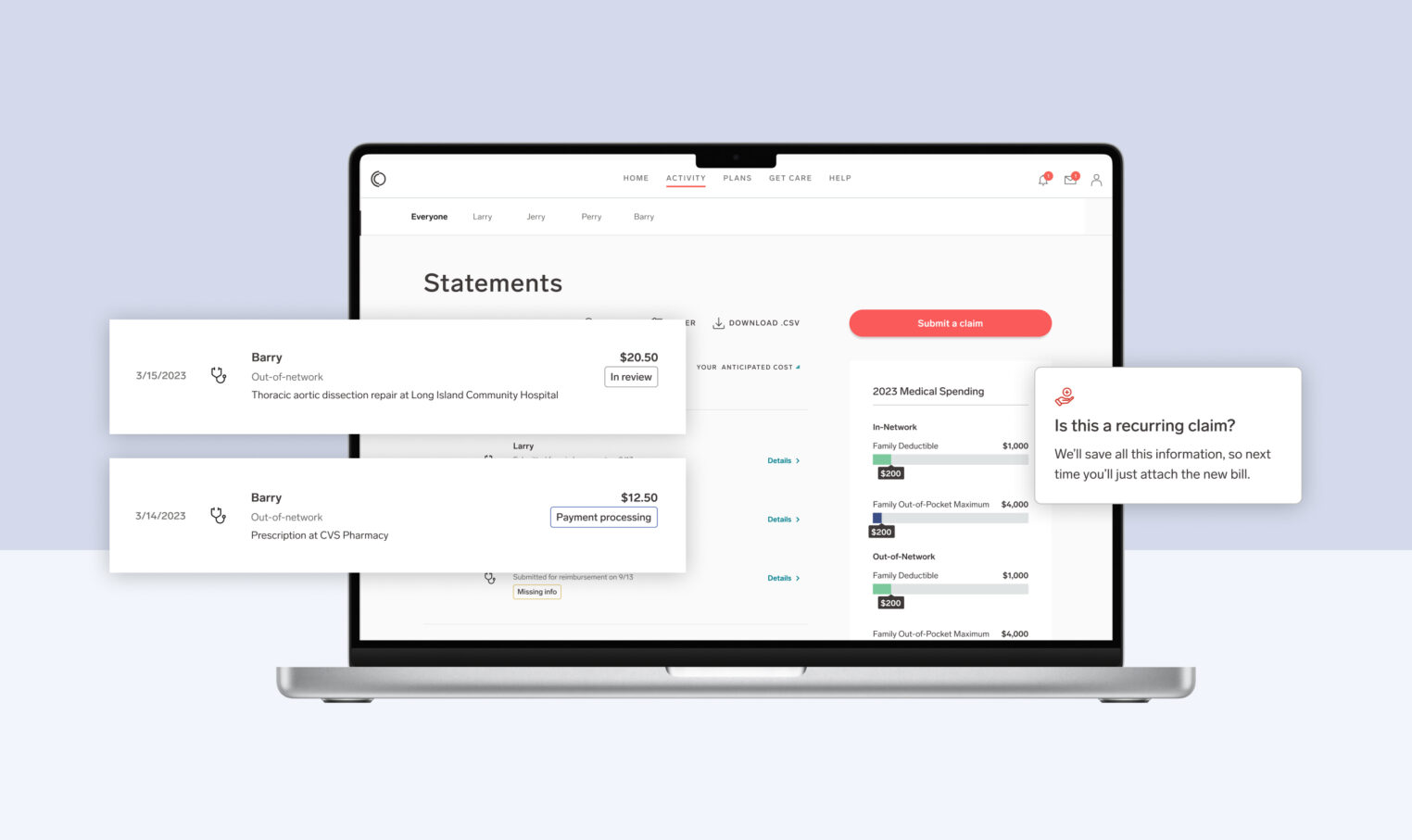
(re)Build around the member
Our healthcare system feels like it was built for the 0.1 percent of people who are already healthcare experts. For the other 99.9 percent of us it feels complicated, frustrating, and completely overwhelming. At Collective Health, we don’t expect you to be a healthcare expert. Instead, we’ve (re)built a completely new type of health insurance experience that revolves around what the other 99.9 percent of members want and need.
Here are some great examples of why (re)building around the member matters:
- Our online portals and mobile apps give members one place for everything—all their plans, cards, claims, programs, providers, and support just a click or fingertip away.
- We built custom tools for our Member Advocates so that they can deliver amazing support and answer coverage questions across all health benefits, help explain or troubleshoot any healthcare claim, or connect members to any health programs offered by their employer. And when a member calls in, they get a real human (not a phone tree) who picks up in seconds (not hours).
Fill the gaps
Two core factors drive a lot of brokenness in healthcare: 1) systems aren’t designed to talk to each other (think how hard it is to set up new eligibility feeds), and 2) humans make mistakes (think how much damage an SSN typo can do). We design our products to solve for those problems, not accept them as inevitable.
Here’s an example:
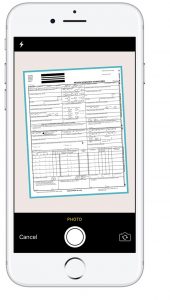
Our members were frustrated with the traditional out-of-network claims submission process. And we don’t blame them—it sucks. Having to fill out an incredibly confusing form, fax it into your network carrier (likely at a FedEx because who has a fax machine?), and wait for some kind of response in the distant future—not ideal. We knew we could fix this.
Harnessing the power of mobile, this year our members will be able to submit out-of-network claims with the snap of a picture in their Collective Health app. They will simply answer a few easy questions, take a picture of their bill, and send it directly to our team. We’ll handle the rest.
Free the data
While the data may not be perfect, it presents a lot of opportunities. Traditional health insurance infrastructure keeps your data in siloes, limiting what it’s able to teach you and what it can be leveraged for. At Collective Health, we break down the walls. As the single platform for all of your data—medical, pharmacy, dental, and vision claims, member engagement, health program utilization, and spending accounts—our technology integrates and normalizes your health benefits information to make your health plan smarter.
Here’s what that looks like:
- Live claims dashboard gives you and your consultant a real-time, integrated view of your population’s medical, pharmacy, dental, and vision claims
- Predictive analytics and machine learning help you connect the right members to the right programs at the right time. Learn more here!
- One system to send (and troubleshoot) eligibility files to all your partners, automatically receive and reconcile partner invoices, and automatically process verified-accurate payment amounts
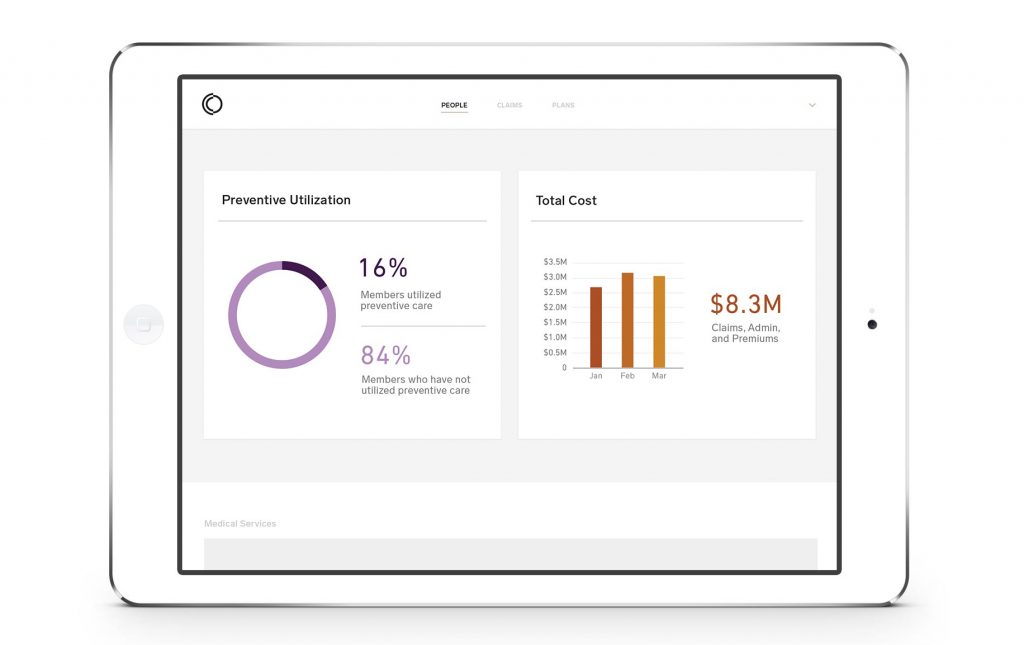
Imagine running your benefits with live data, not six month old reports
Create the standard
In today’s benefits landscape, every new opportunity requires a new set of expensive, fickle integrations. We have a different vision, where a single, robust integration provides access to a growing ecosystem of partnerships and client opportunities.

Imagine a world where all your eligibility, claims, payments, and member communications are running on a single data backbone. When we set standards, everything that should ‘just work’ actually just works, and employers are able to invest in real innovations, instead of just running in place.
Bottom line—technology will sink or save healthcare. At Collective Health, we think that the old systems and old technology aren’t good enough. We’re rebuilding everything about how healthcare works so that together, we can take better care of your people and your business.
Want to learn more about partnering with Collective Health? Join CEO Ali Diab in our on-demand webinar for an overview of the Collective Health platform.