By Ali Diab and Rajaie Batniji
Nearly six years ago, we founded Collective Health with a very personal mission: to make it effortless to navigate, understand, and pay for healthcare. Since then, our mission has become a movement, with a growing number of progressive companies challenging the status quo and adopting our solution. More than 200,000 members across the U.S. depend on us every day to simplify and guide them through the most complex and frustrating parts of our healthcare system: how to understand where you can go, who you can see, what procedures cost, and which procedures are covered when you need help.

Today, we announced that we have raised over $200M in additional funding to accelerate the next phase of our growth, further validating our product. U.S. employers are ready to demand better from their massive annual employee healthcare spend ($1.2T to be exact). Our experience confirms that. Over the last several years, we’ve seen our list of clients evolve from early adopters to a diverse, mainstream set of companies including Pinterest, Restoration Hardware, Red Bull, Zendesk, and more.
And demand is only increasing from employers across the U.S. This funding will help us to meet that opportunity by growing our product, engineering, and sales teams in San Francisco, Chicago, and Lehi, UT, and building new partnerships with innovative health insurers, healthcare systems, and digital health companies.
What’s next for our product
The last several decades have delivered remarkable clinical innovations in genomics, oncology, and the management of many chronic diseases. Similarly, just about every other part of the American enterprise has software companies like Slack, Salesforce, and Workday that have simplified and instrumented how organizations work. Yet there remains a gaping hole in how we navigate and pay for healthcare in the U.S.—where we still depend on fax machines, spreadsheets, and stamps.
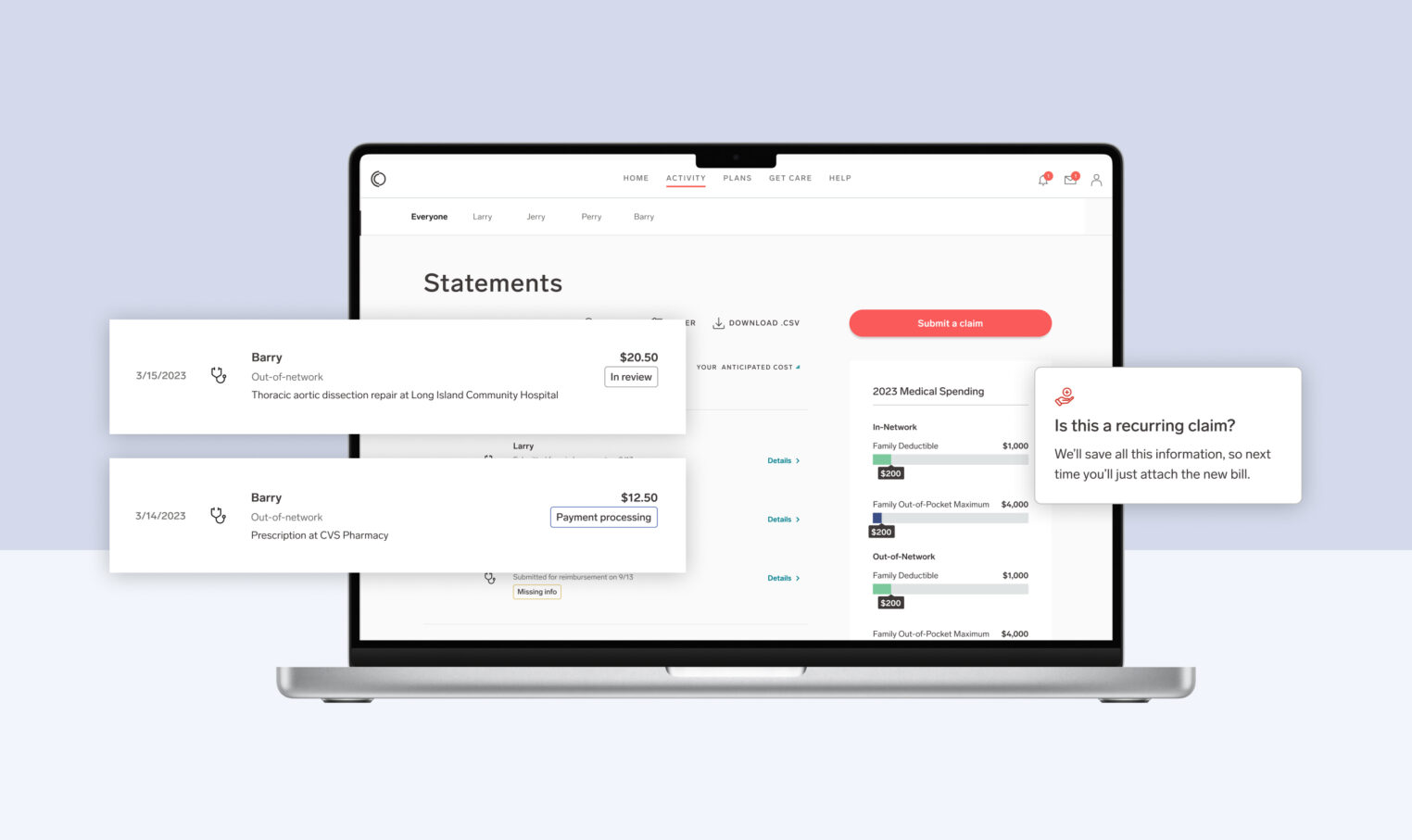
We are obsessed with changing that. Our platform takes employers and members out of the land of spreadsheets and fax machines for a 21st-century experience. It allows employers to take control of their benefits offerings, take better care of their people, and—finally—manage their investment. To continue driving towards our mission, our team is focused on building products that will:
- Reduce administrative burden and waste. Our claims and payments technology aims to enable transparency around how much procedures and doctors visits cost, speed payments, and improve member navigation. As a result, our employer clients and members alike can make more timely, informed healthcare decisions and receive the information they need—right when they need it.
- Drive better outcomes and help to reduce costs. We’re enabling employers to create a seamless experience for their people and drive engagement with a growing ecosystem of new programs and solutions, from behavioral health apps to new solutions to address chronic conditions like diabetes. We’ll continue expanding CH Cortex™, our machine-learning engine, to proactively identify member needs—from chronic disease management to radiology services and beyond—to help guide people to partners, facilities, and benefits.
- Deliver insights that improve population health. It’s critical that employers understand where their healthcare investment is going and its impact on overall workforce health. We’ll continue to build out Collective Health Insights so employers can proactively manage—and improve—population health.
While we’re relentlessly building the next era of technology that improves our system, we never forget that our focus must be on the members we support during some of the most important, and often difficult, moments of their lives. We consider building the experience we want our friends and family to have to be a privilege. Whether we’re helping people to understand coverage for a new cancer diagnosis or supporting them through a high risk pregnancy, we won’t stop until we get it right.
Thank you to our team, our clients, our partners, and to everyone else who has been a part of our movement for getting us this far. We’re looking forward to the next chapter.
— Ali and Rajaie